Supine REM sleep is a phenomenon where an individual experiences obstructive sleep apnea (OSA) while sleeping on their back during the rapid eye movement (REM) stage of sleep. OSA is a sleep-related breathing disorder that causes frequent arousals, leading to fragmented sleep and a loss of restorative function. The supine position further exacerbates OSA by promoting upper airway collapse, making individuals more susceptible to obstructive apneic events. This effect is particularly prominent during REM sleep, where respiratory events tend to be longer and more desaturating compared to non-rapid eye movement (NREM) sleep. The prevalence of supine REM sleep OSA is higher in women than in men and is often associated with mild to moderate OSA severity.
The impact of supine REM sleep OSA has been the subject of extensive research. Studies have found associations between supine REM sleep OSA and various health complications, including systemic hypertension, metabolic abnormalities, and increased cardiometabolic risk. Treatment options for supine REM sleep OSA include continuous positive airway pressure (CPAP) therapy, oral appliances, and lifestyle interventions such as weight loss and exercise. However, patient compliance with CPAP therapy has been a challenge due to the need for prolonged nightly use, often exceeding the recommended minimum of 4 hours per night. As a result, alternative treatments, such as oral appliances and lifestyle changes, have shown some promise in managing supine REM sleep OSA.
| Characteristics | Values |
|---|---|
| Prevalence | Between 17% and 74% |
| Gender | More common in women than in men |
| Severity | Occurs with decreasing frequency from mild to severe OSA |
| Sleep Quality | No association with poor sleep quality |
| Sleepiness | No association with daytime sleepiness |
| Quality of Life | No association with poor quality of life |
| Insomnia | No association with subjective insomnia |
| Obesity | More frequent in obese than non-obese patients |
| Cardiovascular Disease | Associated with systemic hypertension |
| Age | More frequent in young to middle-aged patients |
What You'll Learn
- Supine position and REM sleep in obstructive sleep apnea
- Supine sleep during Polysomnography and the diagnosis of obstructive sleep apnea
- REM sleep obstructive sleep apnea
- The sleep supine position and optimal nasal continuous positive airway pressure
- Supine OSA is the dominant phenotype of the OSA syndrome

Supine position and REM sleep in obstructive sleep apnea
Supine position and REM sleep are both associated with obstructive sleep apnea (OSA). OSA is a sleep-related breathing disorder characterised by complete or partial upper airway obstruction during sleep, resulting in respiratory arousals, sleep fragmentation, and oxygen desaturation. The supine position worsens OSA by promoting upper airway collapse, and this influence is thought to be greater during REM sleep than non-REM sleep.
During REM sleep, the supine position is associated with an increased frequency of apneas and hypopneas. These breathing abnormalities are more common in the supine position due to the increased collapsibility of the airway, particularly at the level of the soft palate and epiglottis. This is further exacerbated by changes in the control of breathing, which favour less stable ventilation when sleeping on the back.
The impact of the supine position on OSA has been studied using the Cartwright index, which defines OSA severity as at least doubling in the supine position or during REM sleep. However, this traditional definition does not consider the time spent in these specific sleep situations, which can lead to clinical bias. A modified Cartwright index has been proposed to address this limitation and better identify borderline cases.
The avoidance of the supine position during sleep can be an effective behavioural strategy to reduce the frequency of apneas and hypopneas, improve sleep quality, and reduce daytime sleepiness in patients with OSA. Treatments such as vibrotactile warning devices have been developed to help patients avoid sleeping on their backs. Additionally, a supine alarm device combining auditory and vibrational signals has been found to increase REM sleep in patients with OSA and improve subjective sleep quality.
In clinical practice, the absence of supine sleep during polysomnography (PSG) can reduce the odds of an OSA diagnosis. Therefore, it is recommended that sleep laboratory policies encourage patients to achieve some supine sleep during PSG to facilitate the diagnosis and subsequent treatment of OSA.
Exploring the Link Between REM Sleep and Depression
You may want to see also

Supine sleep during Polysomnography and the diagnosis of obstructive sleep apnea
The supine position worsens obstructive sleep apnea (OSA) by promoting upper airway collapse. As a result, patients may avoid sleeping on their backs to mitigate OSA's effects. However, avoiding supine sleep during polysomnography (PSG) can lead to a missed OSA diagnosis. This is because the supine position increases the apnea-hypopnea index (AHI), which is used to diagnose OSA.
A study by Dandan et al. (2018) examined the association between the presence/absence of supine sleep and OSA diagnosis during PSG. They found that adult patients suspected of OSA who did not sleep in the supine position during PSG had a significantly lower odds ratio of being diagnosed with OSA compared to those who did sleep in the supine position. This association remained even after adjusting for confounders such as age, body mass index (BMI), and coronary heart disease (CHD).
The avoidance of the supine position may represent a form of self-treatment to reduce the severity of OSA. However, it is important to note that the absence of supine sleep during PSG can reduce the odds of an OSA diagnosis. Therefore, sleep laboratory policies should consider incorporating protocols that encourage patients to sleep in the supine position during PSG to facilitate OSA diagnosis.
Furthermore, it is worth noting that the supine position during sleep makes an individual more susceptible to obstructive apneic events, particularly during rapid eye movement (REM) sleep. A study by Gieselmann and Pietrowsky (2018) found that a supine alarm device combining an auditory and vibrational signal to discourage patients with OSA from sleeping in the supine position resulted in a significant increase in REM sleep compared to a control condition.
Polysomnography and Obstructive Sleep Apnea
Polysomnography (PSG) is a test used to diagnose OSA. It involves monitoring various physiological parameters during sleep, including brain activity, eye movement, muscle activity, heart rate, and breathing patterns. The apnea-hypopnea index (AHI) or respiratory disturbance index (RDI) is calculated based on the number of apneas and hypopneas per hour of sleep, with an AHI of more than five events per hour considered abnormal.
PSG is traditionally performed in a sleep laboratory, but portable devices have emerged that can measure similar sleep variables at home. However, there are challenges in assessing the diagnostic efficacy of in-home PSG compared to in-lab PSG due to the lack of a gold standard for OSA diagnosis.
In summary, supine sleep during PSG is important for the diagnosis of OSA as it increases the AHI, which is a key parameter in diagnosing OSA. The avoidance of the supine position may be a form of self-treatment for OSA, but it can also result in a missed diagnosis. Sleep laboratories should consider implementing protocols to encourage patients to sleep in the supine position during PSG to facilitate OSA diagnosis.
Brain Activity and Infant Movement During REM Sleep
You may want to see also

REM sleep obstructive sleep apnea
Obstructive sleep apnea (OSA) is a highly prevalent sleep-related breathing disorder that causes frequent arousals during the night, resulting in fragmented sleep and a loss of restorative function. The supine position during sleep increases an individual's susceptibility to OSA. This influence of sleeping position is generally greater during rapid eye movement (REM) sleep than in non-rapid eye movement (NREM) sleep stages.
The traditional definition of supine position and REM dependence in OSA states that the severity of OSA is at least doubled when the individual is in the supine position during REM sleep. However, the lack of consideration of the time spent in this particular sleep situation can lead to clinical bias.
A study by Dandan A. et al. (2018) found a statistically significant relationship between the absence/presence of supine sleep during polysomnography (PSG) and the diagnosis of OSA. Patients suspected of OSA who did not achieve supine sleep during PSG had significantly lower odds of being diagnosed with OSA compared to those who did. This finding highlights the importance of encouraging patients to sleep in the supine position during PSG to facilitate an accurate diagnosis of OSA.
A supine alarm device combining an auditory and vibrational signal to discourage patients with OSA from sleeping in the supine position has been found to be effective in improving sleep quality and increasing REM sleep duration. This device resulted in fewer respiratory events, higher baseline blood oxygenation, and fewer oxygen desaturations.
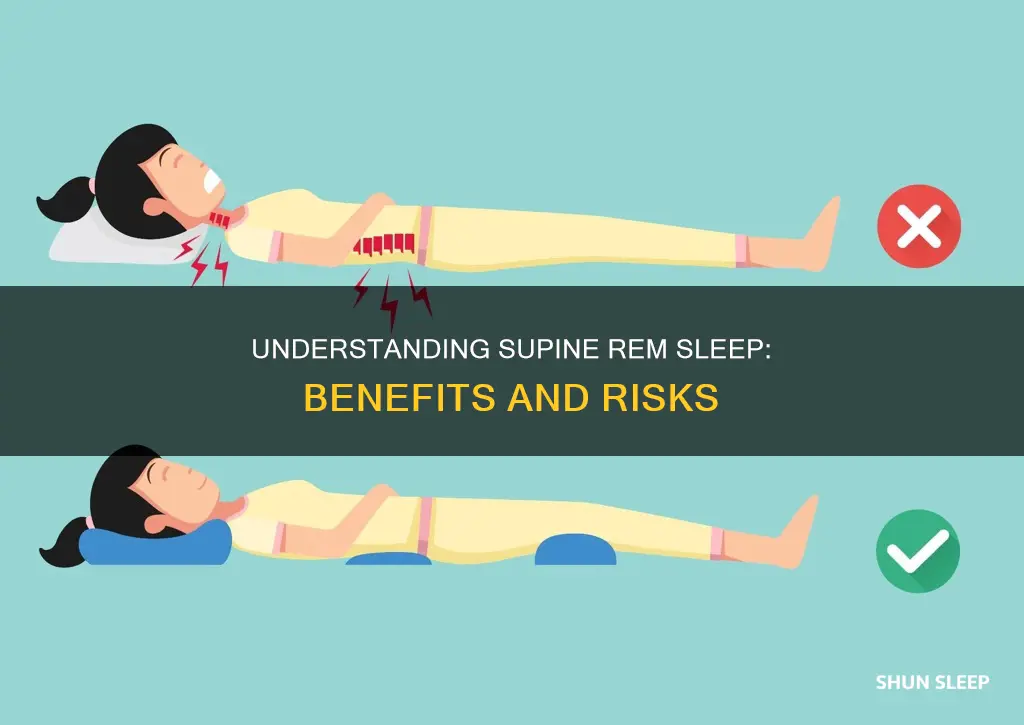
To improve OSA symptoms, individuals can also make changes to their sleep positioning, such as sleeping on their side or stomach, as these positions reduce apnea severity and snoring. Elevating the head of the bed while sleeping on the back can also help reduce the severity of OSA.
Sleep Cycles: Light, Deep, and REM Sleep Harmony
You may want to see also

The sleep supine position and optimal nasal continuous positive airway pressure
Supine REM sleep refers to the rapid eye movement (REM) stage of sleep that occurs when an individual is lying flat on their back. During REM sleep, the individual experiences increased brain activity, dreaming, and muscle relaxation. Obstructive sleep apnea (OSA) is a sleep disorder characterised by disrupted breathing during sleep, often caused by the collapse of the upper airway. The supine position can worsen OSA by promoting upper airway collapse, leading to reduced airflow and oxygen levels.
The sleep supine position has a significant impact on optimal nasal continuous positive airway pressure (nCPAP) in patients with OSA. nCPAP is a treatment for OSA that involves delivering pressurised air through the nose to keep the airway open during sleep. The optimal nCPAP level is crucial for effectively managing OSA and improving sleep quality.
A study by Oksenberg et al. (1999) found that for most OSA patients, the optimal nCPAP level was significantly higher when they slept in the supine position compared to the lateral position. This was consistent across different variables, including REM and non-REM (NREM) sleep, body mass index (BMI), respiratory disturbance index (RDI), and age. The authors recommended that nCPAP titration should not be considered complete unless the patient has slept in the supine position during REM sleep, as this was when the highest nCPAP levels were observed.
The supine position's effect on optimal nCPAP can be attributed to several factors. Firstly, the supine position promotes upper airway collapse, increasing the severity of OSA. Additionally, during REM sleep, there is a reduction in muscle tone, which can further compromise airway stability. The combination of these factors likely contributes to the higher nCPAP requirements in the supine position.
Furthermore, the avoidance of the supine position during sleep studies or polysomnography (PSG) can lead to an underdiagnosis of OSA. Dandan et al. (2018) found that adult patients suspected of OSA who avoided the supine position during PSG had significantly lower odds of receiving an OSA diagnosis. This highlights the importance of encouraging patients to sleep in the supine position during diagnostic procedures to facilitate accurate OSA diagnosis and subsequent treatment.
In summary, the sleep supine position significantly impacts optimal nCPAP levels in OSA patients, with higher pressures required in the supine position to counteract the increased risk of upper airway collapse. This knowledge is essential for tailoring OSA treatments and improving patient outcomes.
Prozac and REM Sleep: What's the Interference?
You may want to see also

Supine OSA is the dominant phenotype of the OSA syndrome
The supine position is associated with more severe and frequent obstructive respiratory events, with over half of OSA patients exhibiting supine-related OSA. This is due to factors such as unfavorable airway geometry, reduced lung volume, and the inability of airway dilator muscles to adequately compensate during airway collapse. The supine position also increases the risk of central sleep apnea-Cheyne Stokes respiration and treatment-emergent central sleep apnea.
The treatment of supine-related OSA is often overlooked in major clinical guidelines, but it can be managed through continuous positive airway pressure, oral appliances, weight loss, or simply by avoiding the supine posture. Encouraging patients to sleep in a supine position during polysomnography can help facilitate OSA diagnosis and subsequent treatment.
Understanding REM Sleep: Frequency and Its Importance
You may want to see also
Frequently asked questions
REM sleep stands for rapid eye movement sleep. It is a sleep stage characterised by low-amplitude, mixed-frequency electroencephalographic activity, general muscle atonia and episodic sequences of rapid eye movements.
Supine REM sleep is when an individual is lying flat on their back during REM sleep.
Supine REM sleep can make individuals with obstructive sleep apnea more susceptible to obstructive apnoeic events.
Supine alarm devices can be used to discourage patients with obstructive sleep apnea from lying in the supine position during sleep.
Symptoms of obstructive sleep apnea include frequent arousals during the night, snoring, witnessed breathing pauses during sleep, sleepiness, and fatigue.
The Cartwright index is a traditional definition used to refer to supine position and REM dependence in obstructive sleep apnea. It states that the severity of obstructive sleep apnea is at least doubled in the corresponding position or sleep stage.