Sleep-wake disturbances are disruptions in the natural sleep-wake cycle, which can significantly impact an individual's overall health and well-being. These disturbances can manifest in various ways, such as difficulty falling asleep, frequent awakenings during the night, early morning awakenings, or excessive daytime sleepiness. They can be caused by a multitude of factors, including lifestyle choices, certain medical conditions, medications, and environmental factors. Understanding the causes and effects of sleep-wake disturbances is crucial for developing effective strategies to improve sleep quality and overall health.
What You'll Learn
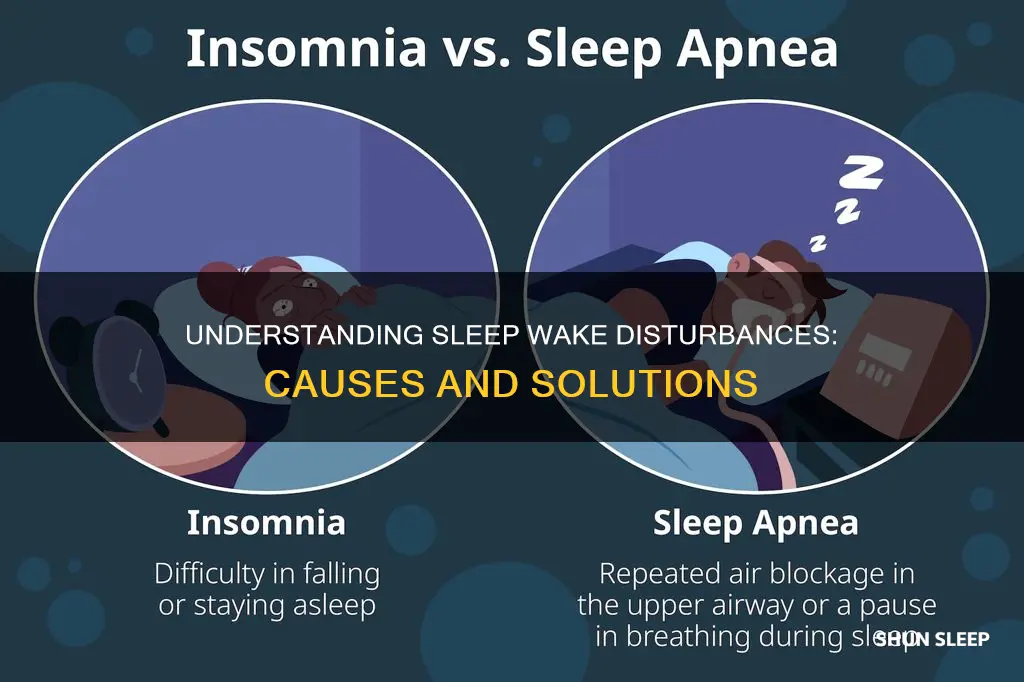
- Insomnia: Difficulty falling asleep despite being tired, often due to stress or medical conditions
- Sleepwalking: A sleep disorder where people walk or perform other activities while still asleep
- Narcolepsy: Excessive daytime sleepiness and sudden muscle weakness, often due to brain disorders
- Sleep Apnea: Breathing interruptions during sleep, causing snoring, gasping, and disrupted sleep
- Shift Work Sleep Disorder: Difficulty sleeping and waking due to irregular work schedules

Insomnia: Difficulty falling asleep despite being tired, often due to stress or medical conditions
Insomnia is a common sleep disorder characterized by the persistent difficulty in falling asleep, despite feeling tired. It is a widespread issue that affects a significant portion of the population, often impacting overall health and quality of life. This condition can be a result of various factors, including stress, medical conditions, and lifestyle choices. Understanding the causes and implementing appropriate strategies can help individuals manage and overcome insomnia effectively.
Stress is a major contributor to insomnia. When faced with stressful situations or chronic anxiety, the body's natural relaxation response may be impaired, making it challenging to unwind and prepare for sleep. Stress-related insomnia can lead to a cycle of worry, where the individual becomes increasingly anxious about not being able to fall asleep, further exacerbating the problem. This type of insomnia often requires stress management techniques such as meditation, deep breathing exercises, or cognitive-behavioral therapy to address the underlying causes and improve sleep quality.
Medical conditions can also play a significant role in causing insomnia. Certain illnesses or health issues can directly impact sleep patterns. For example, chronic pain, respiratory disorders, or gastrointestinal problems may disrupt sleep due to discomfort or the need to frequently visit the bathroom. Additionally, conditions like depression, anxiety disorders, or even the side effects of medications can contribute to insomnia. Managing these medical conditions through appropriate treatment and medication adjustments can help alleviate sleep disturbances.
Lifestyle factors are another crucial aspect to consider. Irregular sleep schedules, excessive caffeine consumption, or exposure to bright screens before bedtime can disrupt the body's natural sleep-wake cycle. Establishing a consistent sleep routine, limiting caffeine intake, and creating a relaxing bedtime environment can significantly improve insomnia symptoms. It is also essential to address any underlying sleep disorders, such as sleep apnea or restless leg syndrome, which may require medical intervention.
In managing insomnia, it is beneficial to maintain a sleep diary to track patterns and identify potential triggers. This can help individuals and healthcare providers develop personalized strategies. Treatment options may include cognitive-behavioral therapy for insomnia (CBT-I), which focuses on changing negative thought patterns and improving sleep hygiene. Additionally, relaxation techniques, such as progressive muscle relaxation or mindfulness practices, can aid in calming the mind and preparing the body for rest. Seeking professional guidance is essential to ensure that any underlying medical conditions are addressed and to receive tailored advice for managing insomnia effectively.
Reviving Brother L2350: Tips to Wake Up Your Printer from Deep Sleep
You may want to see also

Sleepwalking: A sleep disorder where people walk or perform other activities while still asleep
Sleepwalking, also known as somnambulism, is a sleep disorder that falls under the category of sleep-wake disturbances. It is a complex phenomenon that occurs during the sleep cycle, typically in the early stages of non-rapid eye movement (NREM) sleep. During a sleepwalking episode, an individual may appear to be awake and moving around, often performing complex actions such as walking, sitting up, or even engaging in more intricate activities like dressing or going to the bathroom. However, they are still in a state of sleep and are not fully conscious.
This disorder is more common in children, affecting around 15-30% of kids, but it can also occur in adults, especially those with a family history of the condition. Sleepwalkers often have no memory of their nocturnal adventures, which can be quite distressing for both the individual and their caregivers. The episodes usually last for a few minutes to half an hour and may occur several times a night.
The exact cause of sleepwalking is not fully understood, but it is believed to be a combination of genetic and environmental factors. It is often associated with a lack of sleep, certain medications, or underlying sleep disorders such as insomnia or sleep apnea. Emotional stress, fever, or alcohol consumption can also trigger sleepwalking episodes. During these episodes, the individual's brain is highly active, and they may respond to their surroundings, but their muscles are paralyzed, preventing them from acting out their dreams.
Managing sleepwalking involves ensuring a good sleep environment, maintaining a consistent sleep schedule, and addressing any underlying sleep disorders. In some cases, a doctor might prescribe medication to help regulate sleep patterns. It is essential to keep the individual safe during these episodes by ensuring the bedroom is free of potential hazards and by supervising them to prevent any accidents.
Understanding sleepwalking is crucial for both the affected individual and their caregivers. It requires patience, understanding, and sometimes professional guidance to manage this sleep disorder effectively. With proper care and awareness, individuals with sleepwalking can lead healthy lives, ensuring their nocturnal adventures do not interfere with their daily routines.
Uncover the Secrets: Waking the Sleeper Agent from Blackout Slumber
You may want to see also

Narcolepsy: Excessive daytime sleepiness and sudden muscle weakness, often due to brain disorders
Narcolepsy is a neurological disorder characterized by excessive daytime sleepiness and sudden muscle weakness, often due to brain disorders affecting the regulation of sleep-wake cycles. It is a chronic condition that can significantly impact an individual's daily life and functioning. People with narcolepsy experience an overwhelming urge to sleep during the day, even when they have had sufficient nighttime sleep. This excessive sleepiness can lead to a lack of energy, difficulty concentrating, and impaired performance in various aspects of life, including work, education, and social activities.
The primary symptom of narcolepsy is the sudden onset of muscle weakness, known as cataplexy. This can manifest as a loss of muscle tone, often resulting in a collapse or a fall. Cataplexy episodes can be triggered by strong emotions such as laughter, surprise, or anger, and they may vary in intensity and frequency among individuals. For example, a person with narcolepsy might experience a brief period of limpness or a full-body collapse during a surprising event. These episodes can be distressing and may cause embarrassment or social anxiety.
The underlying cause of narcolepsy is often related to brain disorders that disrupt the normal functioning of the sleep-wake regulatory centers in the brain. One of the most common conditions associated with narcolepsy is a deficiency in the neurotransmitter hypocretin (also known as orexin). Hypocretin is produced by specific neurons in the brain and plays a crucial role in regulating sleep and wakefulness. A lack of hypocretin is often linked to the development of narcolepsy, especially in cases where the condition is caused by an autoimmune response or an infection affecting the brain.
Diagnosing narcolepsy involves a comprehensive evaluation, including a detailed medical history, sleep studies, and neurological examinations. Sleep studies, such as polysomnography, help rule out other sleep disorders and assess sleep patterns. A multiple sleep latency test (MSLT) is commonly used to measure the likelihood of falling asleep during the day, which is a key indicator of narcolepsy. This test involves taking short naps at regular intervals throughout the day while monitoring brain activity and muscle tone.
Treatment for narcolepsy aims to manage symptoms and improve the quality of life. Stimulant medications are often prescribed to promote wakefulness during the day. These medications can help reduce excessive sleepiness and improve alertness. Additionally, certain antidepressants and anti-seizure drugs may be used to control cataplexy episodes. Lifestyle modifications, such as maintaining a consistent sleep schedule, regular exercise, and a healthy diet, can also contribute to better sleep-wake regulation. It is essential for individuals with narcolepsy to work closely with healthcare professionals to find the most effective treatment plan for their specific needs.
Fitbit Versa's Wake-Up Feature: Does It Work in Light Sleep?
You may want to see also

Sleep Apnea: Breathing interruptions during sleep, causing snoring, gasping, and disrupted sleep
Sleep apnea is a sleep-related breathing disorder characterized by repeated interruptions in breathing during sleep, often causing snoring, gasping, and disrupted sleep patterns. This condition can significantly impact an individual's quality of life and overall health. During an apnea event, the airway becomes partially or completely blocked, leading to a temporary cessation of airflow. This disruption triggers an automatic arousal from deep sleep, causing the person to wake up briefly to resume breathing.
The most common type of sleep apnea is obstructive sleep apnea (OSA), which occurs when the muscles in the throat relax and block the airway during sleep. This relaxation causes the soft palate and tongue to collapse, narrowing or blocking the airway. As a result, the individual may snore loudly, and these snoring sounds are often accompanied by pauses in breathing. These pauses can last for several seconds and may occur 30 times or more per hour, leading to frequent awakenings and fragmented sleep.
Central sleep apnea, on the other hand, is less common and involves a malfunction in the brain's signaling to the muscles that control breathing. This type of apnea is often associated with other medical conditions, such as heart disease or stroke. Central sleep apnea can also cause snoring and gasping for air but is typically characterized by a lack of snoring sounds before the breathing interruptions.
The impact of sleep apnea on an individual's sleep quality is significant. The frequent awakenings and disrupted sleep cycles can lead to excessive daytime sleepiness, affecting concentration, productivity, and overall cognitive function. Over time, chronic sleep apnea can contribute to various health problems, including hypertension, heart disease, stroke, and metabolic disorders.
Diagnosing sleep apnea involves a comprehensive evaluation, often starting with a sleep study. During the study, patients wear a portable device that monitors their breathing, heart rate, and body movements while sleeping. This data helps healthcare professionals identify the frequency and severity of apnea events and determine the appropriate treatment options. Treatment for sleep apnea may include lifestyle changes, such as weight loss and avoiding alcohol before bed, or the use of continuous positive airway pressure (CPAP) therapy, which involves wearing a mask that delivers pressurized air to keep the airway open during sleep.
Revive Your Laptop: Quick Tips to Wake from Sleep Mode
You may want to see also

Shift Work Sleep Disorder: Difficulty sleeping and waking due to irregular work schedules
Shift Work Sleep Disorder (SWSD) is a common issue for individuals who work non-traditional hours, such as night shifts or rotating schedules. It occurs when the body's natural circadian rhythm, which regulates sleep-wake cycles, is disrupted due to the irregularity of work hours. This disorder can lead to significant difficulties in falling asleep and staying awake during desired times, impacting overall health and quality of life.
The core issue with SWSD is the misalignment between the body's internal clock and the external environment. During the day, our bodies naturally prepare for sleep as the sun sets, and we release melatonin, a hormone that induces sleepiness. However, for shift workers, this natural process is often interrupted. When working night shifts, individuals are exposed to light and noise at unusual hours, which can suppress melatonin production and delay sleep onset. This disruption can lead to a delayed sleep phase, where the body's natural sleep cycle is shifted, making it challenging to fall asleep at conventional bedtime.
Symptoms of SWSD can include excessive daytime sleepiness, difficulty concentrating, irritability, and a general lack of energy. These symptoms can affect work performance, personal relationships, and overall well-being. Individuals with SWSD may experience a constant state of fatigue, making it hard to stay alert during work hours, especially when dealing with complex tasks. Moreover, the disorder can lead to an increased risk of accidents and errors, particularly in safety-critical industries.
To manage SWSD, several strategies can be employed. Firstly, maintaining a consistent sleep schedule is crucial. Despite the irregular work hours, individuals should try to go to bed and wake up at the same time every day, even on days off. This helps to regulate the body's internal clock. Secondly, creating a relaxing bedtime routine can signal to the body that it's time to wind down. This might include activities like reading, light stretching, or listening to soothing music. Additionally, exposure to natural light during the day and avoiding bright screens before bed can help reset the circadian rhythm.
In some cases, medical interventions may be necessary. Doctors might prescribe sleep aids or suggest cognitive-behavioral therapy to help individuals manage their sleep patterns. It is essential for shift workers to prioritize sleep hygiene and seek professional advice if the disorder significantly impacts their lives. While SWSD can be challenging, understanding the underlying causes and implementing appropriate strategies can lead to improved sleep quality and overall better health for those with irregular work schedules.
Troubleshooting: Can't Wake PC from Sleep Mode? We've Got You Covered!
You may want to see also
Frequently asked questions
Sleep wake disturbances, also known as sleep-wake disorders, refer to a group of conditions that affect an individual's ability to fall asleep, stay asleep, or maintain a healthy sleep-wake cycle. These disturbances can significantly impact overall health and quality of life.
Sleep wake disturbances can be caused by various factors, including genetics, lifestyle choices, and underlying medical conditions. Some common causes include sleep apnea, narcolepsy, insomnia, restless leg syndrome, and shift work sleep disorder. Stress, anxiety, and depression can also disrupt sleep patterns.
Treatment for sleep wake disturbances often involves a combination of approaches. This may include behavioral changes such as improving sleep hygiene, establishing a consistent sleep schedule, and practicing relaxation techniques. In some cases, medication or therapy can help manage symptoms. For example, continuous positive airway pressure (CPAP) therapy is used for sleep apnea, while stimulant medications may be prescribed for narcolepsy.
Untreated sleep wake disturbances can lead to a range of health issues. These may include chronic fatigue, decreased cognitive function, impaired concentration, mood disorders, and an increased risk of accidents. Over time, sleep deprivation can contribute to obesity, diabetes, cardiovascular problems, and a weakened immune system.