REM sleep is characterised by rapid eye movements, cortical activation, vivid dreaming, and skeletal muscle paralysis or REM atonia. The brainstem, forebrain, and hypothalamus are involved in the generation and maintenance of REM sleep. The subcoeruleus nucleus (SubC) or sublaterodorsal nucleus is a core region that is active during REM sleep. The activation of these circuits results in low-voltage and fast-wave EEG activity and the suppression of postural motor tone. The cholinergic system is involved in the initiation and control of REM sleep, with cholinergic neurons in the reticular formation and brainstem playing a key role. In contrast, REM sleep is inhibited by serotonergic, noradrenergic, and histaminergic cells. The interaction of these neurotransmitter systems and brain regions leads to the unique features of REM sleep, including muscle paralysis and vivid dreaming.
What You'll Learn

The role of the subcoeruleus nucleus (SubC) in REM sleep
The subcoeruleus nucleus (SubC) is a core region of the brainstem that is active during REM sleep. It is composed of REM-active neurons, with the majority of these cells being glutamatergic, although GABA SubC cells have also been implicated in REM sleep control.
The SubC is hypothesised to regulate REM sleep and its defining features, such as muscle paralysis and cortical activation. REM sleep paralysis is initiated when glutamatergic SubC cells activate neurons in the ventral medial medulla, which causes the release of GABA and glycine onto skeletal motoneurons.
The SubC is also thought to induce REM sleep muscle paralysis by recruiting GABA/glycine neurons in the ventromedial medulla and spinal cord. These cells produce motor atonia during REM sleep by inhibiting skeletal motoneurons.
Pharmacological activation of SubC cells can induce REM sleep motor atonia, while SubC lesions can prevent REM sleep atonia and/or reduce REM sleep amounts.
The SubC is also involved in the control of cataplexy, a sudden and involuntary reduction or loss of skeletal muscle tone during wakefulness. Cataplexy is thought to result from the inappropriate intrusion of REM sleep paralysis into wakefulness.
The subcoeruleus nucleus is therefore a crucial component of REM sleep, playing a key role in regulating muscle paralysis and cortical activation during this sleep stage.
THC and Sleep: Does It Affect Your REM?
You may want to see also

The relationship between REM sleep and dreaming
REM sleep is a unique sleep phase in humans and other mammals, characterised by random rapid eye movements, low muscle tone, and the likelihood of the sleeper to dream vividly. The transition to REM sleep brings about marked physical changes, including electrical bursts known as "ponto-geniculo-occipital waves" (PGO waves) originating in the brainstem. The brainstem and hypothalamus are believed to play a crucial role in regulating REM sleep, with the former being responsible for generating the PGO waves that induce rapid eye movements.
REM sleep is also referred to as "paradoxical sleep" due to its similarities to wakefulness. While the body is paralysed, the brain remains active, with cerebral neurons firing at a similar intensity to that observed during wakefulness. This results in low-amplitude, fast brainwaves that resemble the patterns seen during wakefulness, including theta and gamma waves. The brain's energy consumption during REM sleep equals or even surpasses that of wakefulness, with higher glucose metabolism and oxygen utilisation.
The experience of dreaming is intimately linked to REM sleep. Awakening sleepers during the REM phase is a common method for obtaining dream reports, with individuals typically providing more detailed and narrative descriptions of their dreams. Dreaming during REM sleep is characterised by narrative structure, convincingness, and the incorporation of instinctual themes. The PGO waves that precede rapid eye movements may contribute to the visual aspects of dreams, although a direct relationship remains to be established.
The neural basis of dreaming is not limited solely to REM sleep, as some dreaming can occur during non-REM sleep. However, the distinct neurological aspects of REM sleep, such as the presence of PGO waves and the activation of specific brain regions, suggest a strong association between REM sleep and dreaming.
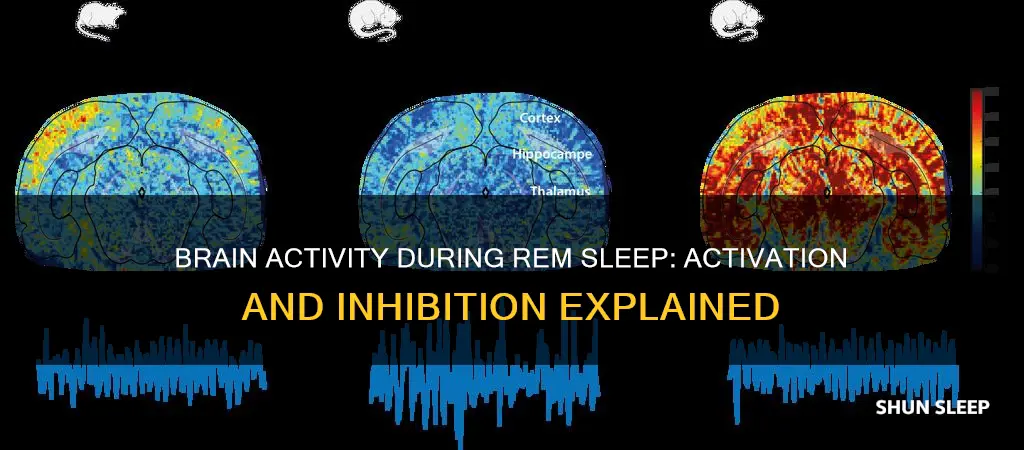
Activation and Inhibition During REM Sleep
The electrical and chemical activity during REM sleep appears to originate in the brainstem, particularly the pontine tegmentum and locus coeruleus. The brainstem circuitry regulating REM sleep involves a complex interplay of neurotransmitter systems, including acetylcholine, monoamines (norepinephrine, serotonin, and histamine), and GABA.
During REM sleep, there is an abundance of the neurotransmitter acetylcholine, combined with a near absence of the monoamine neurotransmitters histamine, serotonin, and norepinephrine. This unique neurochemical milieu during REM sleep contributes to the paradoxical nature of this sleep phase, with higher levels of acetylcholine potentially causing the faster brainwaves observed.
In contrast to non-REM sleep, REM sleep is characterised by the inhibition of motor neurons throughout the body, resulting in REM atonia, or muscle paralysis. This inhibition is achieved through hyperpolarisation of motor neurons, which raises the threshold required to excite them. The medulla oblongata, located between the pons and spine, is believed to play a crucial role in achieving organism-wide muscle inhibition during REM sleep.
The Role of Antidepressants in REM Sleep
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants, have been found to suppress REM sleep. SSRIs decrease dream recall frequency and the proclivity to enter REM sleep, while tricyclic antidepressants, such as imipramine, elicit a homeostatic response in REM sleep similar to that of REM sleep restriction.
In summary, REM sleep is characterised by unique physiological and neurological features that distinguish it from non-REM sleep. The relationship between REM sleep and dreaming is well-established, with dreaming occurring most frequently during REM sleep and being shaped by the distinct brain activity and neurotransmitter systems associated with this sleep phase. The activation and inhibition of specific brain regions and neurotransmitter systems during REM sleep contribute to the paradoxical nature of this sleep phase and provide insights into the subjective experiences that occur during dreaming.
Fitbits: Accurate REM Sleep Trackers or Just a Gimmick?
You may want to see also

The effects of REM sleep deprivation
REM sleep is a unique phase of sleep characterised by random rapid eye movement, low muscle tone, and the likelihood of the sleeper to dream vividly. It is also known as paradoxical sleep due to its similarities to wakefulness. The brain acts as if it is awake during REM sleep, with cerebral neurons firing with the same intensity as in wakefulness.
REM sleep deprivation can have several effects on the body and mind. Here are some of the potential consequences:
- Fatigue: A lack of REM sleep can lead to feelings of fatigue and sleepiness, which can impact work, family life, and activities such as driving.
- Mood and Memory: REM deprivation can cause irritability, changes in mood, and issues with memory and cognition. It may also lead to brief microsleep episodes during the day.
- Health Conditions: Over time, REM sleep deprivation can contribute to various health issues, including obesity, metabolic disorders, type 2 diabetes, cancer, stroke, and neurodegenerative diseases like Alzheimer's. It can also affect cardiovascular health.
- Pain Sensitivity: Studies suggest that REM sleep deprivation can increase sensitivity to pain and reduce the analgesic effects of opioids.
- Psychological Disorders: Mood disorders such as anxiety, depression, and PTSD can be linked to REM sleep deprivation.
- Substance Use: Substance use, including alcohol, cannabis, cocaine, and opioids, can suppress REM sleep.
- Medications: Certain medications, such as opioid painkillers, benzodiazepines, and antidepressants, can affect REM sleep quality and quantity.
- Appetite: REM sleep deprivation may disrupt eating behaviour and increase appetite.
- Aggression: REM sleep deprivation has been linked to increased aggression in laboratory animals.
It is important to note that the long-term effects of REM sleep deprivation are still not fully understood, and more research is needed in this area.
Understanding REM Sleep: The Science Behind Dreaming
You may want to see also

The impact of antidepressants on REM sleep
Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) have different effects on REM sleep. SSRIs, such as paroxetine, citalopram, and fluoxetine, have been found to increase REM sleep latency and suppress REM sleep. This may be due to the activation of serotonergic 5-HT2 receptors and increased noradrenergic and dopaminergic neurotransmission. On the other hand, TCAs like imipramine and doxepin can decrease sleep latency and improve sleep efficiency, increasing slow-wave sleep and having little to no effect on REM sleep.
The impact of antidepressants on sleep also depends on the dose, the time of drug administration, and the duration of treatment. Low doses of sedative antidepressants, such as doxepin and trazodone, can be effective in promoting sleep with fewer side effects. However, these drugs may cause problems in long-term treatment due to oversedation. It is also important to note that the sleep-promoting effects of antidepressants are usually most prominent in the first few weeks of treatment and may persist or aggravate insomnia in some patients.
Additionally, antidepressants can induce or exacerbate certain sleep disorders. For example, SSRIs, SNRIs, and TCAs have been found to disturb the regulation of muscle tone during REM sleep, leading to REM sleep behaviour disorder. Antidepressants that induce weight gain are also contraindicated in patients with sleep apnea.
Further research is needed to determine the specific effects of different classes of antidepressants on REM sleep, as well as the impact of medication doses and administration timing.
Enhancing REM Sleep: Strategies for Deeper Rest
You may want to see also

The impact of REM sleep on memory
REM sleep is a unique sleep phase characterised by random rapid eye movement, low muscle tone, and the likelihood of the sleeper to dream vividly. It is also known as paradoxical sleep due to its similarities to wakefulness. During REM sleep, the brain acts as if it is awake, with cerebral neurons firing with the same intensity as in wakefulness. This phase is associated with an intense neuronal activity, with brain glucose metabolism and oxygen utilisation reaching levels comparable to wakefulness.
REM sleep is important for brain function and is thought to be important for memory. In rats, REM sleep increases following intensive learning, and experimental REM sleep deprivation has been shown to inhibit memory consolidation. In humans, the best evidence for REM's improvement of memory pertains to learning new techniques of problem-solving and new ways of moving the body. REM deprivation has also been shown to impair declarative memory only in more complex cases, such as memories of longer stories.
REM sleep aids the process by which creativity forms associative elements into new combinations that are useful or meet some requirements. This occurs in REM sleep rather than in NREM sleep. Rather than being due to memory processes, this has been attributed to changes during REM sleep in cholinergic and noradrenergic neuromodulation. High levels of acetylcholine in the hippocampus suppress feedback from the hippocampus to the neocortex, while lower levels of acetylcholine and norepinephrine in the neocortex encourage the uncontrolled spread of associational activity within neocortical areas. This is in contrast to waking consciousness, where higher levels of norepinephrine and acetylcholine inhibit recurrent connections in the neocortex.
REM sleep through this process adds creativity by allowing "neocortical structures to reorganise associative hierarchies, in which information from the hippocampus would be reinterpreted in relation to previous semantic representations or nodes."
Alarms and REM Sleep: A Startling Wake-Up Call
You may want to see also
Frequently asked questions
REM sleep, or rapid eye movement sleep, is a unique phase of sleep characterised by random rapid movement of the eyes, low muscle tone throughout the body, and the propensity of the sleeper to dream vividly. It is also known as paradoxical sleep due to its similarities to wakefulness.
During REM sleep, the brain acts as if it is awake, with cerebral neurons firing with the same intensity as in wakefulness. The brainstem and hypothalamus play a role in REM sleep, with the subcoeruleus nucleus (SubC) being the core region active during REM sleep. The REM sleep cycle is controlled by activity of GABAergic neurons in the ventrolateral periaqueductal gray and dorsal paragigantocellular reticular nucleus, as well as melanin-concentrating hormone neurons in the hypothalamus and cholinergic cells in the laterodorsal and pedunculo-pontine tegmentum in the brainstem.
While the body is paralysed during REM sleep, the brain acts as if it is awake, with cerebral neurons firing with the same overall intensity as in wakefulness. In contrast, non-REM sleep is characterised by slow δ (delta) waves.
While the precise function of REM sleep is not well understood, it is thought to aid memory, specifically the preservation of procedural memory, spatial memory, and emotional memory. It may also be important for brain function, as antidepressants that suppress REM sleep are well tolerated.
A lack of REM sleep can cause mild psychological disturbances, such as anxiety, irritability, hallucinations, and difficulty concentrating. It may also have positive consequences, as some symptoms of depression are found to be suppressed by REM deprivation.