Sleep-wake disorders, such as insomnia, hypersomnia, and circadian rhythm sleep-wake disorders, are complex conditions influenced by a combination of genetic, environmental, and biological factors. These disorders can significantly impact an individual's quality of life and overall health. Biological factors play a crucial role in the development and management of these disorders, including the body's natural circadian rhythms, which regulate sleep-wake cycles, and the intricate interplay of neurotransmitters and hormones that influence sleep patterns. Understanding these biological mechanisms is essential for developing effective treatment strategies and promoting better sleep health.
What You'll Learn
- Circadian Rhythm Disruption: External factors like shift work or travel can disrupt natural sleep-wake cycles
- Genetic Predisposition: Certain genes may increase susceptibility to sleep disorders like insomnia or narcolepsy
- Neurotransmitter Imbalance: Altered levels of neurotransmitters like serotonin and GABA can affect sleep quality
- Hormonal Changes: Hormones like cortisol and melatonin play crucial roles in regulating sleep patterns
- Brain Structure Variations: Differences in brain regions like the hypothalamus may contribute to sleep-wake disturbances

Circadian Rhythm Disruption: External factors like shift work or travel can disrupt natural sleep-wake cycles
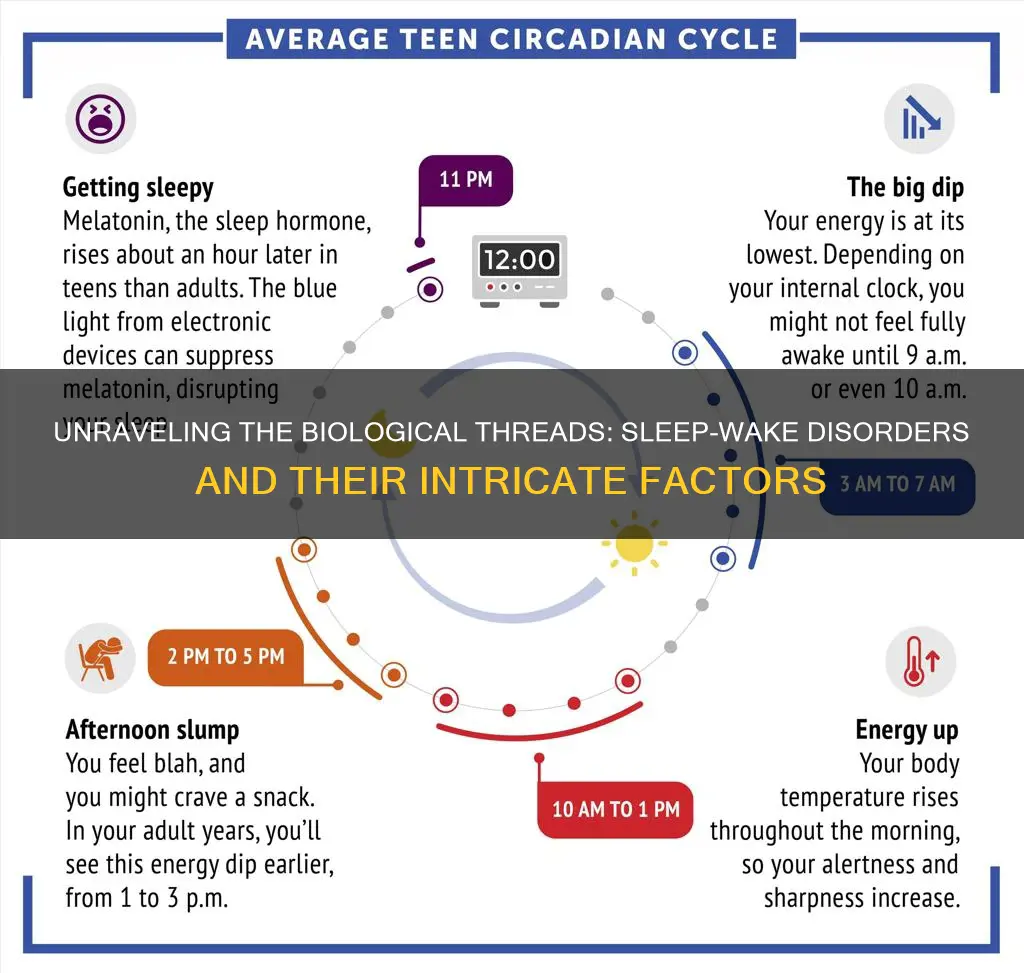
The human body's internal clock, known as the circadian rhythm, is a biological process that regulates various physiological functions, including sleep and wakefulness. This natural rhythm is influenced by external cues, primarily light, and is crucial for maintaining optimal health and performance. However, when this rhythm is disrupted, it can lead to significant sleep-wake disorders, affecting an individual's overall well-being.
One of the primary external factors that can disrupt circadian rhythms is shift work. Individuals who work night shifts or rotating schedules often experience a misalignment between their sleep-wake cycles and the natural day-night cycle. This disruption can result in a phenomenon known as 'social jet lag,' where the body's internal clock is out of sync with the external environment. For example, night shift workers might find it challenging to fall asleep during the day when the sun is shining, and they may feel more alert and energetic at night when they should be resting. This can lead to chronic sleep deprivation, affecting cognitive function, mood, and overall health.
Travel, especially across different time zones, can also significantly impact circadian rhythms. When people travel, their bodies may struggle to adjust to the new light-dark cycles in different locations. This disruption can cause a temporary state of confusion, where individuals experience insomnia or excessive sleepiness, depending on the direction and magnitude of the time zone change. For instance, flying east across multiple time zones can advance the body's internal clock, leading to early awakening and difficulty falling asleep at the desired time. Conversely, traveling west can delay the internal clock, resulting in late-night insomnia and daytime fatigue.
To mitigate the effects of circadian rhythm disruption, several strategies can be employed. Firstly, gradual adjustment is essential before and after shift work or travel. This involves gradually shifting sleep and wake times closer to the desired schedule, allowing the body to adapt. For travelers, gradually adjusting the sleep schedule a few days before and after the trip can help minimize the impact of jet lag. Additionally, maintaining a consistent sleep environment, such as using dim lighting in the evening and bright light during the day, can support the body's natural rhythm.
In conclusion, external factors like shift work and travel can significantly disrupt natural sleep-wake cycles by interfering with the body's circadian rhythm. Understanding these disruptions and implementing strategies to minimize their impact is crucial for maintaining healthy sleep patterns and overall well-being. By recognizing the biological basis of these disorders, individuals can take proactive steps to manage their sleep and improve their quality of life.
Master Your iPhone's Sleep Schedule: Tips for Editing Wake-Up Times
You may want to see also

Genetic Predisposition: Certain genes may increase susceptibility to sleep disorders like insomnia or narcolepsy
The intricate relationship between our genes and sleep health is a fascinating area of study. Research has revealed that certain genetic variations can significantly influence an individual's susceptibility to sleep disorders, particularly insomnia and narcolepsy. These conditions, characterized by persistent difficulties in falling asleep or staying asleep, and excessive daytime sleepiness, respectively, can have a substantial impact on one's quality of life.
Insomnia, for instance, is a complex disorder with a genetic component that can predispose individuals to its development. Studies have identified specific genes associated with insomnia, such as the *MC1R* gene, which plays a role in regulating sleep-wake cycles. Variations in this gene have been linked to an increased risk of insomnia, suggesting that genetic factors can contribute to the likelihood of experiencing chronic sleep difficulties.
Narcolepsy, on the other hand, is a neurological disorder affecting the brain's ability to regulate sleep-wake cycles. It is often associated with the *HLA-DQA1* and *HLA-DQB1* genes, which are part of the human leukocyte antigen (HLA) complex. These genes are crucial for the immune system's function, and certain variants have been consistently found in individuals with narcolepsy, indicating a genetic predisposition to this disorder.
The genetic basis of sleep disorders highlights the importance of personalized approaches to treatment and management. Understanding these genetic predispositions can help healthcare professionals tailor interventions to individual needs. For example, genetic testing could identify individuals at higher risk, allowing for early intervention and prevention strategies. Furthermore, it opens avenues for the development of targeted therapies that address the underlying genetic factors contributing to sleep disorders.
In summary, the genetic predisposition to sleep disorders like insomnia and narcolepsy is a critical biological factor. Identifying specific genes associated with these conditions provides valuable insights into the development of effective treatment strategies. As research in this field progresses, we can expect to see more personalized and precise approaches to managing sleep-wake disorders, ultimately improving the well-being of those affected.
The Mystery of Waking Up Before Death: Unraveling Sleep's Final Moments
You may want to see also

Neurotransmitter Imbalance: Altered levels of neurotransmitters like serotonin and GABA can affect sleep quality
Neurotransmitters are chemical messengers in the brain that play a crucial role in regulating various physiological processes, including sleep. Imbalances in certain neurotransmitters can significantly impact sleep quality and contribute to sleep-wake disorders. One such neurotransmitter is serotonin, which is primarily known for its role in mood regulation but also has a profound effect on sleep.
Serotonin is a precursor to melatonin, a hormone that regulates sleep-wake cycles. Research suggests that individuals with serotonin imbalances may experience disruptions in their melatonin production, leading to difficulties in falling asleep and maintaining restful sleep. Low levels of serotonin can result in insomnia, where individuals struggle to initiate or sustain sleep. This is particularly relevant for those with depression, as serotonin deficiency is a common feature of this disorder, and sleep disturbances are often a symptom.
Another neurotransmitter, gamma-aminobutyric acid (GABA), is an inhibitory neurotransmitter that helps to calm the nervous system and promote relaxation. GABA plays a vital role in modulating sleep by inhibiting the activity of certain brain cells, allowing for a state of calmness and preparing the body for sleep. However, an imbalance in GABA levels can disrupt this process. Increased GABA activity can lead to excessive relaxation, making it challenging to stay awake and alert during the day. Conversely, decreased GABA activity may result in hyperarousal, making it difficult to fall asleep and causing frequent awakenings during the night.
Understanding the relationship between neurotransmitter imbalances and sleep quality is essential for developing effective treatment strategies. For individuals with serotonin or GABA imbalances, specific interventions can be implemented. This may include dietary modifications to increase serotonin production, such as consuming foods rich in tryptophan, which is a precursor to serotonin. Additionally, certain supplements, like magnesium or specific amino acids, can support GABA function. However, it is crucial to consult with healthcare professionals for personalized advice and to ensure that any interventions are safe and appropriate for individual needs.
Unleash the Power: Strategies to Awaken Your Meowth's Potential Before Mount Moon
You may want to see also

Hormonal Changes: Hormones like cortisol and melatonin play crucial roles in regulating sleep patterns
Hormonal changes are a significant aspect of the biological factors that influence sleep-wake disorders. The body's hormonal balance is intricately linked to the regulation of sleep patterns, and disruptions in these hormones can lead to various sleep issues. Two key hormones, cortisol and melatonin, are at the forefront of this regulatory process.
Cortisol, often referred to as the 'stress hormone', is primarily known for its role in the body's stress response. It is typically produced in higher amounts during the day, especially in the morning, to promote alertness and energy. This morning surge of cortisol helps individuals wake up and prepare for the day ahead. However, cortisol levels should naturally decrease in the evening to facilitate the transition into a state of relaxation and sleepiness. When cortisol levels are dysregulated, it can lead to difficulties in falling asleep, as the body may remain in a state of heightened arousal. Chronic stress, for instance, can result in persistently elevated cortisol levels, making it challenging to achieve a calm state conducive to sleep.
Melatonin, on the other hand, is a hormone that primarily regulates the sleep-wake cycle, also known as the circadian rhythm. It is often referred to as the 'sleep hormone' because its production increases in the evening, promoting sleepiness, and decreases in the morning, helping to wake up. This hormone is highly sensitive to light, and its secretion is stimulated by darkness, especially after exposure to bright light during the day. In the absence of light, the body produces more melatonin, signaling that it's time to prepare for sleep. Disruptions in melatonin production can lead to sleep disorders. For example, individuals with delayed sleep phase disorder often have a delayed release of melatonin, causing them to feel sleepy later in the evening and struggle to wake up in the morning.
The intricate relationship between cortisol and melatonin is essential for maintaining a healthy sleep-wake cycle. When cortisol levels are appropriate, it helps prepare the body for sleep by reducing arousal and promoting relaxation. As cortisol levels drop in the evening, melatonin production increases, further enhancing the sleep drive. This harmonious interplay ensures that individuals can fall asleep at night and feel rested in the morning. However, when this balance is disrupted, it can result in sleep disorders, such as insomnia or hypersomnia, where individuals either have difficulty falling asleep or experience excessive sleepiness during the day.
Understanding the role of these hormones in sleep-wake disorders can provide valuable insights into the treatment and management of such conditions. Strategies to address hormonal imbalances, such as stress management techniques, light therapy, or specific dietary adjustments, can help restore the natural balance of cortisol and melatonin, thereby improving sleep quality and overall well-being.
Understanding Sleep: Why Some People Don't Wake Up
You may want to see also

Brain Structure Variations: Differences in brain regions like the hypothalamus may contribute to sleep-wake disturbances
The brain's intricate architecture plays a pivotal role in regulating sleep-wake cycles, and variations in specific regions, particularly the hypothalamus, can significantly impact an individual's ability to maintain a healthy sleep-wake rhythm. The hypothalamus, a small but highly significant structure deep within the brain, serves as the body's command center for sleep and wakefulness. It is responsible for integrating a myriad of signals from various systems, including the circadian rhythm, the body's internal clock that regulates daily activities.
One of the key functions of the hypothalamus is the production of orexins, also known as hypocretins, which are neurotransmitters that promote wakefulness. These orexins are released by a subset of neurons in the hypothalamus and play a critical role in maintaining alertness and attention. Individuals with sleep-wake disorders, such as narcolepsy, often exhibit a significant loss of orexin-producing neurons, leading to excessive daytime sleepiness and sudden sleep attacks. This discovery has been instrumental in understanding the biological basis of narcolepsy and has opened new avenues for treatment.
Beyond its role in wakefulness, the hypothalamus is also involved in the regulation of sleep stages. It helps modulate the transition between different sleep cycles, including rapid eye movement (REM) sleep and non-REM sleep. During sleep, the hypothalamus releases certain hormones and neurotransmitters that influence the brain's activity, ensuring a cyclical pattern of sleep and wakefulness. Disruptions in this process can lead to fragmented sleep patterns and contribute to sleep-wake disorders.
Research has revealed that structural variations in the hypothalamus can be associated with sleep-wake disturbances. For instance, studies have shown that individuals with insomnia may have a smaller volume of the hypothalamus compared to healthy controls. This finding suggests that the hypothalamus's size and functionality could be a biological marker for sleep disorders. Additionally, differences in the connectivity and activity of hypothalamic neurons might contribute to the development of sleep-wake disorders, providing a more nuanced understanding of these complex conditions.
Understanding the role of brain structure variations, especially in the hypothalamus, offers valuable insights into the biological underpinnings of sleep-wake disorders. This knowledge can pave the way for more targeted and effective treatments, potentially involving neurostimulation techniques or specific pharmacological interventions that aim to restore the normal functioning of the hypothalamus and, consequently, improve sleep quality and overall well-being.
The Eternal Dilemma: Keats or Sleep, Which to Choose?
You may want to see also
Frequently asked questions
Sleep-wake disorders, such as insomnia, hypersomnia, and circadian rhythm sleep-wake disorders, are influenced by various biological factors. These include the body's internal clock, or circadian rhythm, which regulates the sleep-wake cycle. Disruptions to this rhythm can lead to conditions like delayed sleep phase disorder, where individuals fall asleep and wake up later than usual, or advanced sleep phase disorder, where sleep and wake times are earlier than normal. Additionally, the brain's production of neurotransmitters, such as GABA and serotonin, plays a crucial role in regulating sleep. Imbalances in these chemicals can affect the quality and timing of sleep.
Environmental factors significantly influence sleep-wake disorders. Exposure to light, especially during the evening, can disrupt the body's natural production of melatonin, a hormone that regulates sleep. This is why maintaining a consistent sleep schedule and minimizing exposure to bright lights before bedtime is essential. Additionally, the presence of noise or an uncomfortable sleep environment can interfere with sleep quality. External factors like temperature, humidity, and air quality can also impact sleep, as they may affect an individual's comfort and ability to fall asleep or stay asleep.
Yes, genetic factors can play a role in the development of sleep-wake disorders. Certain genetic variations have been associated with an increased risk of insomnia, sleep apnea, and other sleep disorders. For example, a genetic predisposition to insomnia may affect the regulation of sleep-wake cycles, making it challenging for individuals to fall asleep or maintain restful sleep. Additionally, genetic factors can influence the body's sensitivity to environmental cues, such as light and temperature, which are crucial for maintaining a healthy sleep-wake rhythm. Understanding the genetic basis of sleep disorders can help in developing personalized treatment approaches.