REM sleep, or rapid eye movement sleep, is the sleep stage during which people dream the most. Usually, people enter REM sleep after about 60 to 90 minutes of falling asleep. However, people with narcolepsy, a chronic neurological disorder, can enter REM sleep much faster, sometimes within 15 minutes of falling asleep. This means that people with narcolepsy can start dreaming almost immediately after falling asleep.
| Characteristics | Values |
|---|---|
| Time taken to enter REM sleep | 15 minutes or less for people with narcolepsy; 60-90 minutes for people without narcolepsy |
What You'll Learn
- REM sleep is reached within 15-20 minutes of falling asleep
- Cataplexy: sudden muscle weakness caused by strong emotions
- Hallucinations: vivid, frightening, and multi-sensory
- Sleep paralysis: temporary loss of muscle control
- Disrupted sleep: difficulty staying asleep due to vivid dreams, breathing problems, or body movements

REM sleep is reached within 15-20 minutes of falling asleep
REM sleep is typically reached about 60 to 90 minutes after falling asleep. However, people with narcolepsy can enter REM sleep within 15 to 20 minutes of falling asleep. Narcolepsy is a chronic neurological disorder that affects the brain's ability to control sleep-wake cycles. People with narcolepsy may feel rested after waking but then feel very sleepy throughout the day. They also experience fragmented sleep at night, meaning they can't stay asleep for long periods.
Narcolepsy is characterised by overwhelming and persistent daytime sleepiness, or "sleep attacks". These sleep attacks can occur at any time during any activity and can be extremely disruptive to daily life. People with narcolepsy often have lower quality of life and may miss out on important milestones such as graduation due to the disorder. It can also impact their employment opportunities and driving capabilities.
The sleep disorder can present in two types: Type 1 and Type 2. Type 1 narcolepsy is characterised by the sudden onset of muscle weakness in response to strong emotion, known as cataplexy. This can cause the head to bob or legs to give out while the patient is awake. People with Type 1 narcolepsy also have lower levels of hypocretin, a chemical in the brain that regulates sleep and wakefulness. Type 2 narcolepsy does not involve cataplexy and is harder to diagnose. People with Type 2 narcolepsy have normal hypocretin levels and less severe symptoms.
Narcolepsy is typically diagnosed through a polysomnogram (PSG) or a multiple sleep latency test (MSLT). A PSG is an overnight test that measures brain activity, muscle movements, breathing, and eye movements during sleep. An MSLT is a daytime test that measures how quickly a person falls asleep and whether they enter REM sleep. If a person enters REM sleep within 20 minutes, it may indicate narcolepsy.
While there is no cure for narcolepsy, treatments can help manage symptoms and improve quality of life. Stimulants and antidepressants are commonly prescribed to promote wakefulness and tackle hallucinations, sleep paralysis, and cataplexy. Lifestyle changes, such as maintaining a regular sleep schedule, avoiding caffeine and alcohol, and exercising regularly, can also help improve sleep quality.
Niquil's Impact: Enhancing REM Sleep or Just a Myth?
You may want to see also

Cataplexy: sudden muscle weakness caused by strong emotions
Cataplexy is a sudden and brief loss of muscle control triggered by strong emotions such as laughter, excitement, anger, or fear. It is a common symptom of type 1 narcolepsy, a chronic sleep disorder characterized by excessive daytime sleepiness and sleep paralysis. During a cataplexy attack, individuals remain conscious but experience temporary paralysis, ranging from a slight drooping of the eyelids to a total body collapse.
Laughter is the most common trigger of cataplexy, but other emotions such as excitement, anger, surprise, fear, or stress can also trigger attacks. These attacks usually last from a few seconds to a couple of minutes and can occur anywhere from a few times a year to several times a day. While cataplexy attacks are not typically dangerous, they can be scary and disrupt daily activities.
The underlying cause of cataplexy is believed to be related to the loss of neurons that produce hypocretin (also known as orexin), a neurotransmitter that promotes wakefulness and regulates sleep-wake cycles. People with narcolepsy type 1 have significantly lower levels of hypocretin, which leads to a disruption in the regulation of sleep and wakefulness. This results in a mix of sleep and wakefulness elements, with individuals experiencing muscle weakness or dream activity of REM sleep while they are awake.
There is no cure for cataplexy, but it can be managed through medication and lifestyle changes. Medications such as wake-promoting agents, antidepressants, and sodium oxybate can help reduce the frequency and intensity of attacks. Lifestyle changes, including maintaining a consistent sleep schedule, avoiding caffeine and alcohol before bed, and regular exercise, can also help improve sleep quality and reduce the number of cataplexy attacks.
It is important for individuals experiencing cataplexy to work closely with their healthcare team to find the right combination of treatments and to ensure their safety and well-being. Additionally, joining support groups and educating loved ones about cataplexy attacks can provide emotional support and help others understand what the individual is going through.
Flexeril and Sleep: Safe Combination?
You may want to see also

Hallucinations: vivid, frightening, and multi-sensory
During normal sleep, people enter REM sleep after about 60 to 90 minutes. However, people with narcolepsy can enter REM sleep much faster, often within 15 minutes of falling asleep. This can cause them to experience vivid hallucinations as they fall asleep or when they are waking up. These hallucinations are known as hypnagogic hallucinations.
Hypnagogic hallucinations are vivid experiences that can be quite intense and realistic. They can involve visual, auditory, or physical sensations. For example, a person may see moving patterns and shapes, or vivid images of faces, animals, or scenes. They may hear voices or music, or feel physical sensations such as falling or weightlessness. In some cases, they may sense the presence of another person in the room, even when no one is there.
These hallucinations can be frightening, especially when they occur alongside sleep paralysis, where a person is temporarily unable to move or speak while falling asleep or waking up. This can last for several minutes, during which the person remains fully conscious but unable to speak or move. The hallucinations that accompany sleep paralysis can be very vivid and sometimes frightening, involving multiple senses such as sight, sound, or touch.
Hypnagogic hallucinations are a common symptom of narcolepsy, but they can also occur in people without the disorder. They are generally considered harmless and are not usually a cause for concern. However, if they significantly impact daily life, it may be a good idea to consult a doctor.
Seroquel's Effect on REM Sleep: What You Need to Know
You may want to see also

Sleep paralysis: temporary loss of muscle control
Sleep paralysis is a temporary loss of muscle control that occurs during the rapid eye movement (REM) stage of the sleep cycle. During REM sleep, the body experiences temporary muscle paralysis, known as atonia, which prevents dreams from being acted out. While standard REM sleep involves vivid dreaming along with atonia, both typically end when a person wakes up. However, in sleep paralysis, the atonia and mental imagery of REM sleep persist even after a person becomes conscious and awake.
During a sleep paralysis episode, an individual is aware of their surroundings but unable to move or speak. They may still move their eyes and breathe, and the episode can last from a few seconds to up to 20 minutes, with an average length of around six minutes. Sleep paralysis is often associated with hallucinations, which can be frightening and involve the perception of a dangerous presence in the room or sensations of suffocation.
The exact cause of sleep paralysis is unknown, but it is linked to sleep disorders and certain mental health conditions. It is more common among people with varying sleep schedules and those with underlying mental health conditions such as anxiety, bipolar disorder, or post-traumatic stress disorder (PTSD). Sleep paralysis can be a frightening experience, but it is not considered dangerous. However, frequent episodes can cause emotional distress and impact an individual's daytime functioning.
While there is no treatment to stop a sleep paralysis episode once it starts, certain medications and improvements in sleep hygiene can help reduce the frequency of episodes. Establishing a consistent sleep schedule, creating a comfortable sleep environment, and limiting substance use and electronic device usage before bed can all help improve sleep quality and reduce the occurrence of sleep paralysis.
REM Sleep: A Universal Stage of Sleep?
You may want to see also

Disrupted sleep: difficulty staying asleep due to vivid dreams, breathing problems, or body movements
Disrupted Sleep
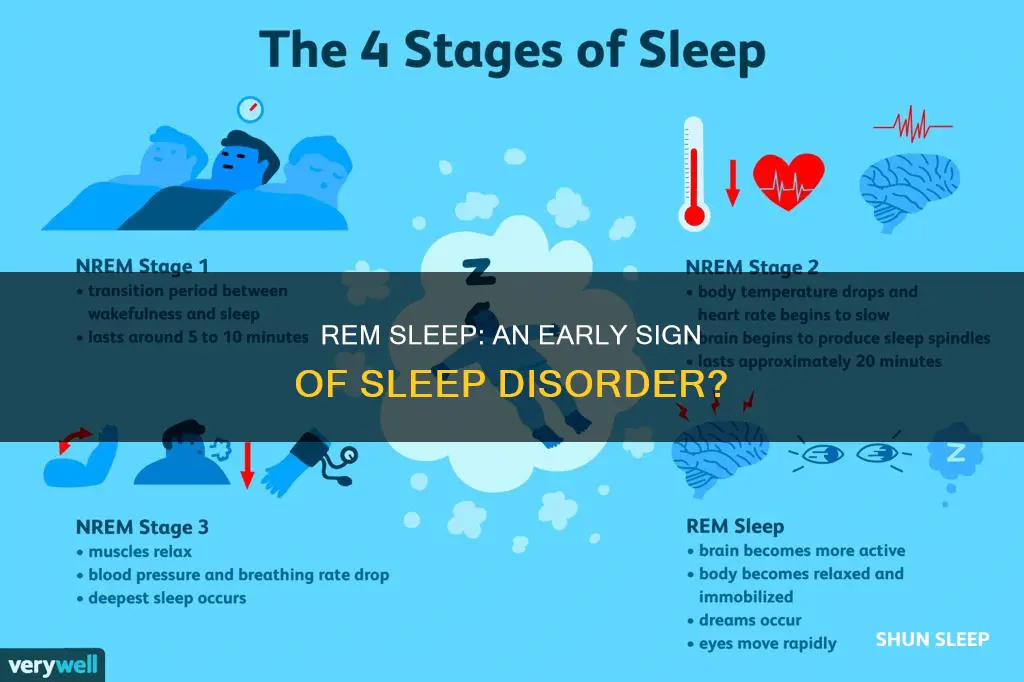
Sleep is divided into two types: REM sleep and non-REM sleep. The latter is further divided into four stages, with the fourth stage being REM sleep, which occurs about 90 minutes after falling asleep. During REM sleep, people dream, and their eyes move rapidly from side to side. Their arm and leg muscles become paralysed, preventing them from acting out their dreams.
However, people with REM sleep behaviour disorder (RBD) do not experience this paralysis. As a result, they might punch, kick, shout, or grab while asleep, disturbing their sleep and that of those around them. RBD can be a standalone problem or a symptom of another neurological disorder, such as narcolepsy.
Vivid Dreams
People tend to spend about two hours each night dreaming. Sleep deprivation, alcohol consumption, and substance use can all lead to vivid dreams. People with narcolepsy tend to enter REM sleep within 15 minutes of falling asleep, resulting in vivid dreams even during brief naps.
Breathing Problems
Breathing problems during sleep can be caused by conditions affecting the lungs or heart, such as asthma, allergies, or anxiety. Sleep apnea is a condition that causes narrowed airways and low oxygen levels, leading to disrupted sleep.
Body Movements
Restless leg syndrome is a condition that causes an urge to move the legs while resting, making it difficult to fall asleep. Narcolepsy can also cause body movements during sleep, as people with this condition may experience muscle weakness or dream activity of REM sleep while they are awake.
REM Sleep and Children: What Parents Should Know
You may want to see also
Frequently asked questions
REM stands for "rapid eye movement." It is the sleep stage during which people do the most dreaming. The brain keeps the person's muscles limp during this sleep stage, which prevents them from acting out their dreams.
In a normal sleep cycle, people enter REM sleep after about 60 to 90 minutes. However, people with narcolepsy can enter REM sleep much faster, often within 15 minutes of falling asleep.
The four main symptoms of narcolepsy are excessive daytime sleepiness, sudden muscle weakness (cataplexy), sleep-related hallucinations, and sleep paralysis.
Narcolepsy is typically diagnosed through a combination of a physical exam, medical history, sleep studies (polysomnogram), multiple sleep latency tests (MSLT), and lumbar puncture (spinal tap).
Narcolepsy is uncommon, affecting about 25 to 50 out of every 100,000 people worldwide. However, due to the difficulty in diagnosing this condition, the actual number may be higher.