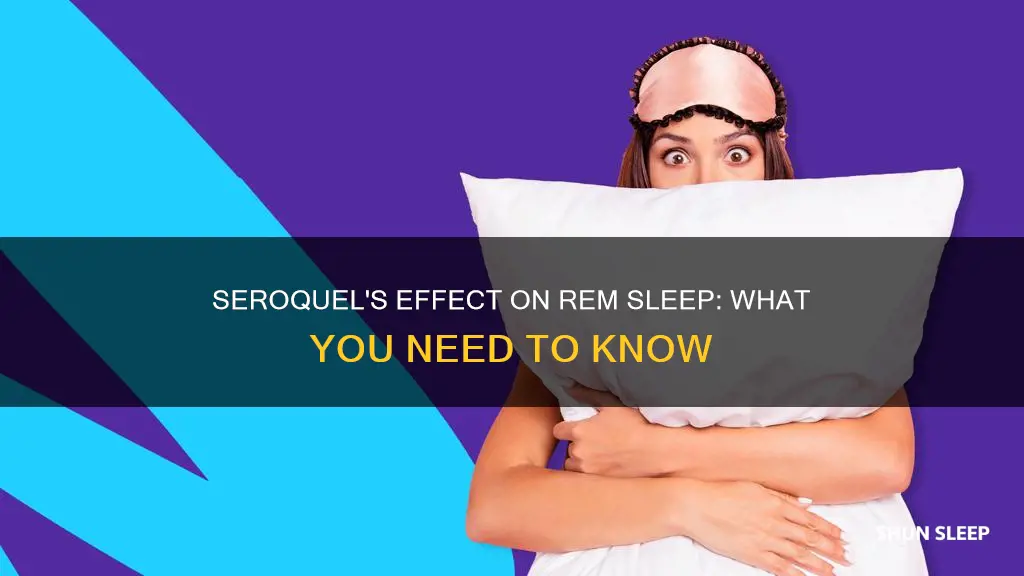
Quetiapine, also known as Seroquel, is an antipsychotic medication approved for the treatment of schizophrenia, bipolar disorder, and as an adjunctive therapy with antidepressants for major depressive disorder. However, it is frequently prescribed off-label for insomnia, anxiety, and agitation at lower doses than those used for its approved indications. Quetiapine affects multiple central nervous system receptors, resulting in a variety of effects, including sedation. While quetiapine has sedative properties and is often prescribed for insomnia, there is limited evidence supporting its efficacy for this use.
Quetiapine has been found to improve sleep in healthy individuals and those with psychiatric disorders, such as bipolar disorder, schizophrenia, and depression. It can reduce sleep latency and increase total sleep time and sleep efficiency. However, it has also been associated with a decrease in rapid eye movement (REM) sleep, which is important for emotional well-being. Additionally, quetiapine has been linked to periodic leg movements and orthostatic hypotension, a drop in blood pressure when moving from a sitting to standing position.
While quetiapine may have some benefits for sleep, it also carries risks and side effects. It is associated with weight gain, metabolic syndrome, and QTc prolongation. It can cause movement disorders such as restless legs syndrome, tardive dyskinesia, and akathisia. Quetiapine has a short half-life, and its pharmacokinetic profile may make it more attractive for abuse, especially when crushed for intravenous injection or intranasal snorting. It is important to note that quetiapine is not recommended as a first-line treatment for insomnia and should be used cautiously, particularly in the elderly and those at risk for QTc prolongation.
What You'll Learn
- Quetiapine is an atypical antipsychotic, approved for treating schizophrenia, bipolar disorder, and major depressive disorder
- Quetiapine is increasingly being prescribed off-label for insomnia, despite a lack of evidence supporting its effectiveness
- Quetiapine affects multiple central nervous system receptors, resulting in a variety of effects, including sedation
- Quetiapine's sedative effects are due to its strong histamine H1 receptor antagonism
- Quetiapine is associated with weight gain and metabolic syndrome

Quetiapine is an atypical antipsychotic, approved for treating schizophrenia, bipolar disorder, and major depressive disorder
Quetiapine, also known by its brand name Seroquel, is an atypical antipsychotic medication. It is approved by the FDA for the treatment of schizophrenia, acute manic episodes, and as an adjunctive treatment for major depressive disorder. It is also used off-label for several indications, including generalized anxiety disorder, insomnia, and chronic post-traumatic stress disorder.
Quetiapine works by changing the activity of certain natural substances in the brain. It is an antagonist for D2 receptors and 5-HT2 receptors, and also acts on 5-HT1A, H1 histamine, and α1-adrenergic receptors.
When used to treat schizophrenia, the recommended dosage of quetiapine for adults ranges from 150 mg to 750 mg per day. For the treatment of acute manic episodes associated with bipolar I disorder, the typical dosage is between 400 mg and 800 mg per day. As an adjunctive treatment for major depressive disorder, the dosage ranges from 50 mg to 300 mg per day.
Quetiapine has been associated with several side effects, including somnolence, dizziness, orthostatic hypotension, weight gain, and dry mouth. It can also cause more serious side effects, such as an increased risk of death in elderly patients with dementia-related psychosis and an increased risk of suicidal thoughts and behavior.
While quetiapine has been used at low doses to aid sleep, studies on its effectiveness for this purpose are limited, and it is not recommended by many doctors as a first-line sleep aid due to its potential side effects. However, it may be prescribed for sleep in people with certain mental health disorders.
Apple Watch and REM Sleep: What's the Connection?
You may want to see also

Quetiapine is increasingly being prescribed off-label for insomnia, despite a lack of evidence supporting its effectiveness
Quetiapine is an antipsychotic medication that is increasingly being prescribed off-label to treat insomnia. However, there is a lack of evidence supporting its effectiveness for this purpose. Quetiapine is approved by the United States Food and Drug Administration (FDA) to treat schizophrenia, major depressive disorder, and bipolar disorder. It is also approved as an adjunctive therapy with antidepressants for major depressive disorder.
Despite its lack of approval for treating insomnia, quetiapine is frequently prescribed off-label for this purpose, particularly at low doses. This is possibly due to a desire to avoid standard medications with known addictive qualities and adverse side effects. Quetiapine has sedative effects, which make it appealing as a sleep aid.
However, there is limited evidence to support the use of quetiapine for insomnia in the general population. Most studies investigating its effectiveness for this purpose have been conducted on small sample sizes or specific populations, such as people with psychiatric disorders or post-traumatic stress disorder (PTSD). While quetiapine may improve sleep in these specific populations, the evidence is inconclusive regarding its effectiveness in the general population.
Furthermore, quetiapine is associated with several side effects, including weight gain, metabolic syndrome, and QTc prolongation. It also carries particular risks for elderly patients, including cognitive decline and an increased risk of cardiovascular events, stroke, and mortality.
Overall, while quetiapine may be useful for improving sleep in specific patient populations, there is insufficient evidence to support its widespread use as a treatment for insomnia. The potential risks and side effects associated with quetiapine should be carefully considered before prescribing it for this purpose.
Otters' Sleep Patterns: Do They Experience REM Sleep?
You may want to see also

Quetiapine affects multiple central nervous system receptors, resulting in a variety of effects, including sedation
Quetiapine, also known as Seroquel, is a second-generation antipsychotic drug. It is approved by the US Food and Drug Administration (FDA) for the treatment of schizophrenia, bipolar disorder, and major depressive disorder. However, it is frequently prescribed off-label, including for insomnia. Quetiapine affects multiple central nervous system receptors, resulting in a variety of effects, including sedation.
The drug works by binding to a wide variety of central nervous system (CNS) receptors. At lower dosages, it primarily affects histaminergic (H1) and alpha 1 and alpha 2 adrenergic receptors, mediating sedative effects. At medium and high doses, it has an additive affinity for serotonergic receptors (5-HT1A, 5-HT2A, 5-HT2B, 5-HT2C) and the dopamine D2 receptors, causing mood stabilization and improvements in anxiety, deep sleep, and psychosis. Quetiapine's sedative effects are thought to arise from its 5-HT2 and H1 receptor blockade capabilities, similar to those of medications used as sedatives.
Quetiapine is often prescribed off-label for insomnia due to its well-known sedative and sleep-promoting effects at low doses. However, evidence supporting its use for insomnia is limited, and it is associated with weight gain, metabolic syndrome, and QTc prolongation. It should be used cautiously and with appropriate monitoring for adverse effects and abuse. The use of quetiapine to treat insomnia should be confined primarily to patients with comorbid mood or schizophrenia spectrum disorders.
Quetiapine's short duration to peak plasma concentration, which is comparable to that of many approved hypnotics, may make it more attractive for abuse. It can also be crushed for intravenous injection or intranasal snorting, or mixed with other drugs of abuse to achieve faster and more intense effects. Quetiapine taken through such routes is associated with an increased risk of neuroleptic toxicity.
Quetiapine is generally regarded as being non-addictive and having a good safety profile. However, its potential for misuse and abuse, along with its cardiometabolic effects, warrant caution for its off-label use. While it may be useful for treating insomnia in patients with comorbid schizophrenia or mood disorders, there is insufficient evidence to support its broad use for treating insomnia in the general patient population.
Scientists Who Uncovered the Mystery of REM Sleep
You may want to see also

Quetiapine's sedative effects are due to its strong histamine H1 receptor antagonism
Quetiapine is an atypical antipsychotic medication indicated for schizophrenia and bipolar disorder. However, due to its sedative effects, it is often prescribed off-label in low doses to treat insomnia. Quetiapine's sedative effects are due to its strong histamine H1 receptor antagonism, which aids in reducing allergic reactions and blocking the vasodilator effects of histamine.
Quetiapine is a strong histamine H1 receptor antagonist, even at low doses of 25 mg. This property is considered the primary reason for its hypnotic and sedative effects. Quetiapine also modulates other wake-promoting and arousal systems, including dopamine, muscarinic acetylcholine, and 5-HT2A–C receptors. It acts as an antagonist to these receptors, further contributing to its sedative effects.
Quetiapine's ability to block histamine H1 receptors results in its hypnotic effects. This property makes it useful for treating insomnia, especially in patients with psychiatric disorders who do not respond to primary or secondary treatments. However, it is not recommended as a first-line treatment for sleep complications due to potential adverse effects, such as periodic leg movements, akathisia, and metabolic complications.
In summary, quetiapine's sedative effects are primarily attributed to its strong histamine H1 receptor antagonism, which aids in reducing allergic reactions and blocking the vasodilator effects of histamine. While this makes quetiapine useful for treating insomnia, particularly in patients with psychiatric disorders, it is not recommended as a first-line treatment due to potential adverse effects.
Understanding REM Sleep: Timing and Its Importance
You may want to see also

Quetiapine is associated with weight gain and metabolic syndrome
Quetiapine is an atypical antipsychotic drug that is known to induce weight gain and other metabolic complications. The underlying mechanisms are multifactorial and poorly understood, with almost no information on the effect of dosage. Quetiapine has been associated with a significant dose-dependent increase in weight gain and a higher risk of clinically relevant weight gain (≥7% from baseline). It has also been linked to an increased risk of hypertriglyceridemia and total and LDL hypercholesterolemia.
The weight gain caused by quetiapine can be a significant barrier to medication adherence, and strategies for managing and reducing the risk of metabolic disturbances should be considered from the outset of treatment. Quetiapine's effect on weight gain and lipid alterations emphasizes the importance of prescribing the minimal effective dose. However, as the effect size of a dose increase on metabolic worsening is low, the potential harm of low-dose quetiapine should not be dismissed. Prescriptions must be carefully evaluated and regularly reviewed in light of side-effect onset.
Quetiapine's weight gain side effect is one of the most problematic adverse effects facing patients with serious mental illness. It increases the risk of metabolic complications and physical ill health and can reduce compliance. Quetiapine is associated with a higher risk of metabolic syndrome, which will increase the risk of diabetes mellitus and cardiovascular illness over the next 5–10 years.
The risk of weight gain appears to be highest in the first year of treatment, so careful monitoring and early intervention are crucial in managing this side effect. Non-pharmacological interventions such as dietary counselling, exercise programs, and cognitive and behavioural strategies can be effective in preventing and treating weight gain caused by quetiapine. Pharmacological interventions such as switching to an alternative antipsychotic with a lower risk of weight gain or adding an adjuvant medication can also be considered.
Alcohol's Effect on Sleep: Postponing REM Sleep?
You may want to see also
Frequently asked questions
Seroquil, also known as Quetiapine, is a second-generation antipsychotic drug. It is approved by the US Food and Drug Administration (FDA) for the treatment of schizophrenia, bipolar disorder, and major depressive disorder.
Quetiapine affects multiple central nervous system receptors, resulting in a variety of effects, including sedation. It can improve sleep latency (reducing the time from being fully awake to falling asleep) and increase total sleep duration and efficiency. However, it may also decrease rapid-eye-movement (REM) sleep.
Seroquil is associated with weight gain, metabolic syndrome, and QTc prolongation. It may also cause extrapyramidal side effects such as restless legs syndrome, tardive dyskinesia, akathisia, and periodic leg movement disorder.
Quetiapine carries risks of abuse and addiction, especially when crushed for intravenous injection or intranasal snorting. It is also associated with metabolic and cardiac complications, including weight gain, increased blood pressure and blood glucose, and development of metabolic syndrome.
Quetiapine should be used cautiously in the elderly due to reduced drug clearance, and it carries a black-box warning from the American Geriatrics Society for increased risk of cardiovascular events, stroke, and overall mortality in this population. It should also be avoided in patients at risk of QTc prolongation and those with a history of substance abuse.
Quetiapine may be useful for treating insomnia in patients with comorbid mood or schizophrenia spectrum disorders. However, it is not recommended as a first-line treatment for insomnia due to its side effect profile and limited evidence of efficacy.