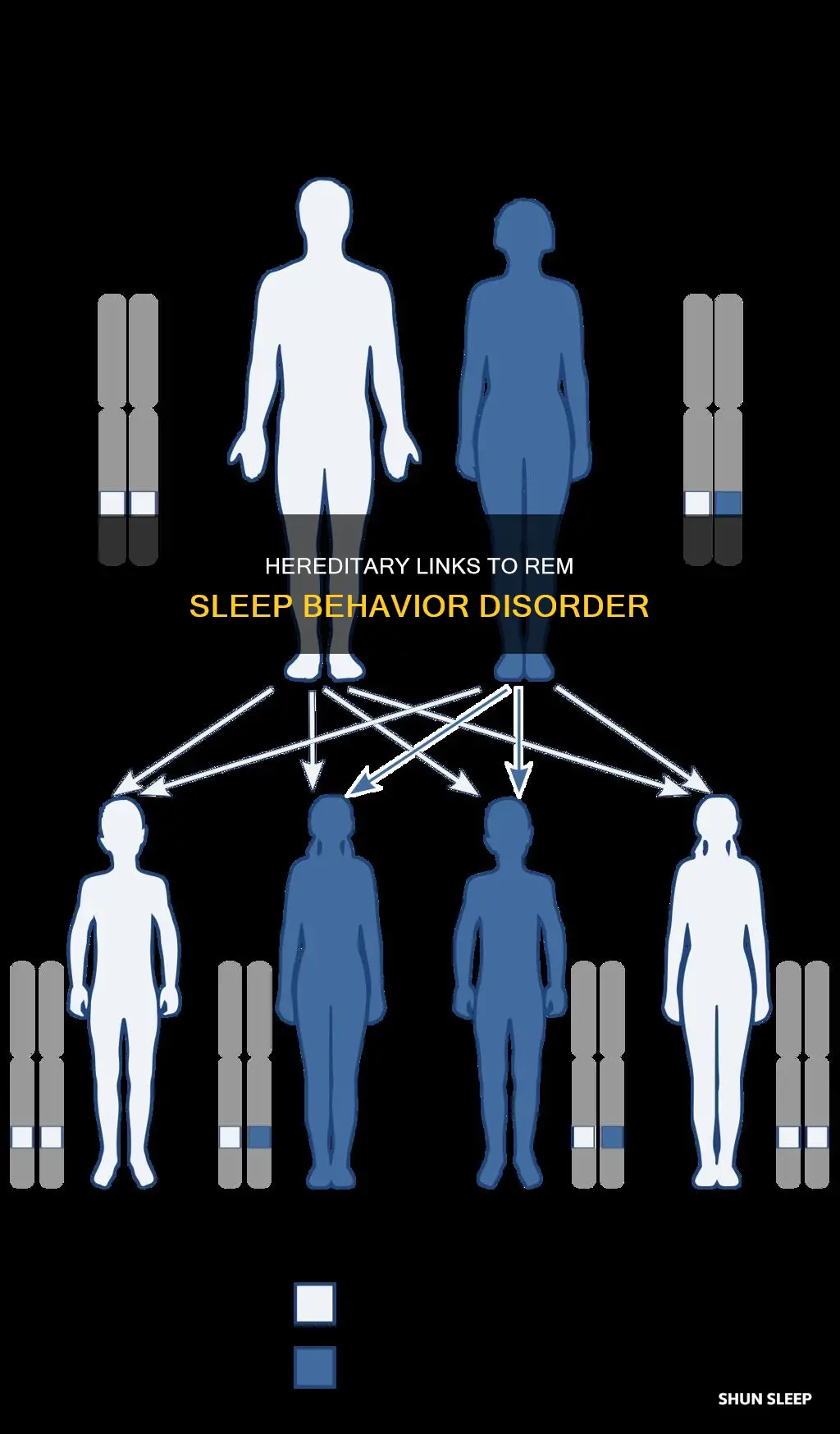
REM sleep behaviour disorder (RBD) is a sleep disorder characterised by the loss of normal muscle atonia during REM sleep, which results in complex motor behaviour while dreaming. Idiopathic RBD is generally considered to be a sporadic condition, but studies have found a positive family history of dream enactment in 13.8% of iRBD cases compared to 4.8% of controls. This suggests the possibility of a genetic contribution to RBD.
| Characteristics | Values |
|---|---|
| Prevalence | 0.38%–0.5% in the general population |
| Age of onset | Typically in elderly persons, but can occur at any age |
| Gender distribution | Predominantly in males |
| Heritability | Suggested by some studies, but not confirmed |
What You'll Learn
- A positive family history of dream enactment was reported in 13.8% of iRBD cases
- REM sleep behaviour disorder (RBD) is characterised by abnormal behaviours associated with dream mentation and loss of REM sleep atonia
- RBD is a strong indicator of more extensive neuropathology in Parkinson's disease
- RBD is a parasomnia strongly linked to synucleinopathies, including Parkinson's disease
- RBD is a sleep disorder characterised by the loss of normal voluntary muscle atonia during REM sleep

A positive family history of dream enactment was reported in 13.8% of iRBD cases
REM sleep behaviour disorder (RBD) is a sleep disorder characterised by the loss of normal muscle atonia during REM sleep, which results in complex motor behaviour while dreaming. Idiopathic RBD (iRBD) is generally considered to be a sporadic condition, but a 2013 study found that a positive family history of dream enactment was reported in 13.8% of iRBD cases, compared to 4.8% of controls. This suggests the possibility of a genetic contribution to RBD.
The study, which was published in the journal 'Neurology', recruited 316 patients with polysomnography-confirmed iRBD from 12 international RBD study group centres. All subjects completed a self-administered questionnaire that collected proxy-reported information on family history of tremor, gait trouble, balance trouble, Parkinson's disease, memory loss, and Alzheimer's disease. The questionnaire also included a single question asking about possible symptoms of RBD among first-degree relatives.
The results showed that a positive family history of dream enactment was reported in 13.8% of iRBD cases, compared to 4.8% of controls. The odds ratio for siblings was 6.1, and for parents, it was 3.2. There was no significant difference in sex, current age, or age at self-reported RBD onset in possible familial vs sporadic iRBD. No differences were found in family history of tremor, walking and balance troubles, Parkinson's disease, memory loss, or Alzheimer's disease.
The study concluded that there is a possible familial component to iRBD, with a significantly higher frequency of a positive family history of presumed RBD among patients with polysomnography-confirmed iRBD compared to controls. This raises the possibility of a genetic contribution to RBD, and further studies are needed to validate these findings.
Newborns' REM Sleep: Shorter Periods, Critical Development
You may want to see also

REM sleep behaviour disorder (RBD) is characterised by abnormal behaviours associated with dream mentation and loss of REM sleep atonia
RBD is typically observed in middle-aged to elderly individuals and is more prevalent in men. While the exact cause of RBD is unknown, it has been linked to degenerative neurological conditions such as Parkinson's disease, multisystem atrophy, and Lewy body dementia. Additionally, certain medications, including antidepressants and alcohol or sedative-hypnotic withdrawal, have been associated with RBD.
RBD is a chronic sleep condition that can pose risks of injury to the affected individual or their bed partner due to violent movements during sleep. The diagnosis of RBD is challenging due to its low prevalence and limited awareness among medical professionals. The gold standard for RBD diagnosis is a combination of clinical assessment and overnight video polysomnography (v-PSG), which involves monitoring brain activity, muscle activity, respiratory function, and other parameters during sleep.
The prognosis for RBD varies depending on its subtype. In some cases, RBD may resolve with the discontinuation of certain medications. However, for individuals with RBD as a secondary condition to neurological lesions or in conjunction with neurodegenerative diseases, the management of RBD becomes a part of their holistic care. While there is no cure for RBD, treatment options include pharmacological interventions, such as clonazepam, and behavioural recommendations to create a safer sleep environment.
REM Sleep: Brain Waves During Wakefulness
You may want to see also

RBD is a strong indicator of more extensive neuropathology in Parkinson's disease
REM sleep behaviour disorder (RBD) is a chronic sleep condition characterised by dream enactment and loss of REM atonia. It is a strong indicator of more extensive neuropathology in Parkinson's disease.
RBD is a prodromal symptom of Parkinson's disease, with up to 90% of patients with RBD eventually developing a neurodegenerative disorder such as Parkinson's disease (PD). RBD can precede the diagnosis of PD by 8 years, and is one of the most specific predictors of the synuclein-mediated neurodegenerative disease. RBD patients also exhibit accelerated disease progression and a more severe phenotype than α-synucleinopathy sufferers without RBD.
The primary pathology of RBD appears to be an excitation/inhibition imbalance in the brainstem nuclei controlling REM muscle tone. This results in abnormal motor behaviours during REM sleep. RBD is associated with changes in multiple neurotransmitter systems, including the cholinergic, noradrenergic, and dopaminergic circuits.
The presence of RBD in patients with PD is associated with a more advanced disease profile, with greater cognitive impairment. RBD is also associated with a poorer prognosis in PD.
HR Monitors: Can They Detect REM Sleep?
You may want to see also

RBD is a parasomnia strongly linked to synucleinopathies, including Parkinson's disease
REM sleep behaviour disorder (RBD) is a parasomnia characterised by violent movements and increased motor activity during REM sleep. It is often associated with neurodegenerative disorders, such as Parkinson's disease (PD) and Lewy body dementia (LBD). RBD is a strong indicator of synucleinopathies, with over 80% of people with RBD going on to develop an overt synucleinopathy.
RBD can be either idiopathic or symptomatic of an underlying neurodegenerative disorder. Longitudinal studies have shown that idiopathic RBD is strongly associated with eventual phenoconversion to a neurodegenerative disease. The risk of phenoconversion is about 15-35% between two and five years, increasing to 41-90.9% if the follow-up period is extended to 12-25 years.
RBD is characterised by the loss of muscle tone and undesired movements from dream enactment in REM sleep episodes. It is different from sleepwalking, which takes place in non-REM and transitional stages of sleep, whereas RBD occurs during REM sleep. People with RBD can be aware of their dream content as they act it out and can recall vivid details of their dreams when they wake up.
RBD is mostly diagnosed in men over 55 years of age but can also affect people taking certain medications, such as antidepressants. It is a potent early biomarker of synucleinopathy, as it is usually diagnosed 5-10 years before PD or LBD. RBD patients are primarily advised to sleep in a built-safe environment to increase sleep quality and reduce the risk of injury to themselves or their bed partners.
REM Sleep: The Intriguing Stage of Our Sleep Cycle
You may want to see also

RBD is a sleep disorder characterised by the loss of normal voluntary muscle atonia during REM sleep
REM sleep behaviour disorder (RBD) is a sleep disorder characterised by the loss of normal voluntary muscle atonia during REM sleep. This loss of muscle atonia is often referred to as REM Sleep without Atonia (RSWA). During normal REM sleep, the body's voluntary muscles are paralysed, but people with RBD act out their dreams through vocalisations and complex motor behaviours.
RBD is associated with vivid dreams, which the sleeper may attempt to act out. This can result in violent movements, which may pose a threat to the sleeper or their bed partner. Anecdotal reports of violent dreams are common, but more systematic studies have found that they make up a small percentage of all RBD events. The sleeper's eyes will remain closed as they engage with the dream environment, and their movements are generally contained to their immediate surroundings. Upon awakening from a large motor event, the RBD individual will be alert and oriented to their surroundings.
The frequency of motor events may vary greatly between individuals with RBD, ranging from multiple episodes per night to one episode per month. In any one patient, the severity and frequency of the behaviours may also vary from night to night, and over the course of their condition. The mechanisms behind this fluctuation are unknown.
RBD is thought to be caused by an excitation/inhibition imbalance in the brainstem nuclei controlling REM muscle tone. Movement during REM sleep is controlled by two systems: one controls the input to spinal cord motoneurons to generate muscle atonia (extrapyramidal), and the other controls motor cortex activation to suppress locomotor activity (pyramidal). The main generator of REM sleep is the predominantly-glutamatergic Subcoeruleus/Pre-Locus Coeruleus complex [SubC/PC], which is situated just below the noradrenergic locus coeruleus in the pons.
RBD may present on its own (idiopathic RBD) or may be secondary to another condition. Idiopathic RBD is often considered to be a sporadic condition, but there is evidence to suggest that it may have a genetic component. A study found a positive family history of dream enactment in 13.8% of iRBD cases compared to 4.8% of controls.
RBD is found to occur, on average, eight years before the presentation of the core motor or cognitive symptoms required for the clinical diagnosis of Parkinson's disease or dementia with Lewy bodies. It is estimated that up to 90% of patients with iRBD will eventually develop one of these synucleinopathies.
Clitoral Erection: REM Sleep's Arousing Mystery
You may want to see also
Frequently asked questions
REM sleep behavior disorder (RBD) is a sleep disorder characterized by the loss of normal muscle atonia during REM sleep. While RBD is considered to be a sporadic condition, a study has found a positive family history of dream enactment in 13.8% of iRBD cases compared to 4.8% of controls. This suggests the possibility of a genetic contribution to RBD.
Individuals with RBD often present to clinics with complaints of injury to themselves or their bed partner due to violent movements during sleep.
The gold-standard protocol for RBD diagnosis is a clinical assessment coupled with an overnight video polysomnography (v-PSG) study.
Clonazepam is the general first-line agent used for the treatment of RBD symptoms.