Elimination disorders, characterized by the sudden and unexplained urge to urinate or defecate, can present unique challenges in the context of sleep-wake disorders. These disorders often disrupt normal sleep patterns and daily routines, leading to significant distress and functional impairment. The question of whether elimination disorders should be classified as sleep-wake disorders is a complex one, as it involves understanding the underlying neurobiological mechanisms and the impact on an individual's overall well-being. This paragraph aims to explore the relationship between elimination disorders and sleep-wake disturbances, considering the potential diagnostic and therapeutic implications.
| Characteristics | Values |
|---|---|
| Definition | Elimination disorders are a group of conditions where individuals intentionally pass urine or feces in inappropriate places, often in response to stress or anxiety. |
| Types | Encopresis (soiling) and Enuresis (bedwetting). |
| Age of Onset | Typically begins in early childhood and may persist into adolescence or adulthood if left untreated. |
| Causes | Stress, anxiety, developmental delays, neurological disorders, and genetic factors. |
| Sleep-Wake Connection | There is a strong association between elimination disorders and sleep-wake disturbances. Bedwetting episodes often occur during the night, disrupting sleep patterns. |
| Treatment | Cognitive-behavioral therapy, desensitization techniques, medication, and environmental modifications. |
| Management | Behavioral interventions, such as bladder training and scheduled voiding, are essential to improve sleep quality and reduce nocturnal accidents. |
| Prognosis | With appropriate treatment, many individuals with elimination disorders can achieve remission and improve their sleep-wake cycles. |
| Differential Diagnosis | Other sleep-wake disorders like nocturnal enuresis, sleep-related movement disorders, and sleep apnea should be considered for accurate diagnosis. |
What You'll Learn
- Definition and Classification: Elimination disorders are sleep-wake disorders characterized by the inability to control urination or defecation
- Symptoms and Diagnosis: Common symptoms include frequent bedwetting and daytime accidents, requiring medical evaluation
- Psychological Factors: Emotional stress, anxiety, and trauma can contribute to the development of elimination disorders
- Treatment Approaches: Behavioral therapy, medication, and lifestyle changes are effective treatment options
- Prognosis and Management: With proper treatment, many individuals can achieve remission and improved sleep quality

Definition and Classification: Elimination disorders are sleep-wake disorders characterized by the inability to control urination or defecation
Elimination disorders, also known as enuresis and encopresis, are indeed classified as sleep-wake disorders within the broader category of neurodevelopmental disorders. These disorders are primarily characterized by the involuntary loss of bladder or bowel control, which can significantly impact an individual's daily life and social interactions. The inability to control these essential bodily functions is a defining feature of these disorders and often leads to distress and embarrassment for those affected.
In the context of sleep-wake disorders, elimination disorders are unique as they involve a disruption in the normal patterns of sleep and wakefulness. Typically, individuals with these disorders experience episodes of incontinence during the night, which can be associated with sleep disturbances. The act of urination or defecation during sleep can disrupt the individual's sleep architecture, leading to fragmented sleep patterns and potential sleep deprivation. This disruption in sleep can further exacerbate the symptoms of the disorder, creating a vicious cycle.
The classification of elimination disorders as sleep-wake disorders is essential for accurate diagnosis and treatment. Healthcare professionals often assess the timing and frequency of these involuntary acts in relation to sleep patterns. For example, nocturnal enuresis (bedwetting) is a common sleep-related issue in children, while adult enuresis may be linked to underlying sleep disorders or stress. Similarly, encopresis, which involves the involuntary soiling of clothing with feces, can also be associated with sleep disturbances, especially in children with developmental delays or gastrointestinal issues.
Understanding the relationship between elimination disorders and sleep is crucial for developing effective management strategies. Treatment approaches often focus on improving sleep hygiene, addressing any underlying sleep disorders, and providing behavioral interventions to enhance bladder and bowel control. Cognitive-behavioral therapy (CBT) is a common therapeutic modality used to help individuals cope with the emotional impact of these disorders and develop strategies to manage their symptoms.
In summary, elimination disorders are a distinct category of sleep-wake disorders characterized by the involuntary loss of bladder or bowel control. Their classification within the sleep-wake disorder spectrum highlights the importance of considering sleep patterns and disturbances in the diagnosis and treatment of these conditions. Recognizing the interplay between elimination disorders and sleep can lead to more comprehensive and effective management strategies for affected individuals.
Revive Your Digestion: Tips to Awaken Your Sleeping Bowels
You may want to see also

Symptoms and Diagnosis: Common symptoms include frequent bedwetting and daytime accidents, requiring medical evaluation
Elimination disorders, often referred to as enuresis, are a group of conditions characterized by the involuntary loss of urine or feces. These disorders can significantly impact a child's quality of life and social interactions, and they often require medical attention and intervention. The symptoms of elimination disorders are primarily related to the involuntary release of bodily fluids, which can manifest in various ways.
One of the most common symptoms is frequent bedwetting, also known as nocturnal enuresis. This occurs when a child wakes up in the morning with wet bedding, despite having voided before going to bed. Bedwetting is often associated with a lack of awareness of the need to urinate, as the brain does not fully develop the ability to control bladder function during sleep. As a result, children with bedwetting may not remember or realize they need to use the bathroom, leading to involuntary urination.
In addition to bedwetting, daytime accidents are another hallmark symptom of elimination disorders. These accidents involve the unintentional release of urine during the day, often when the child is not able to reach a bathroom in time. Daytime accidents can be distressing for both the child and their caregivers, as they may lead to social embarrassment and a fear of using the bathroom independently. The frequency and severity of these accidents can vary, but they often require medical evaluation to determine the underlying cause and develop an appropriate treatment plan.
The diagnosis of elimination disorders typically involves a comprehensive medical evaluation, which may include a thorough medical history, physical examination, and laboratory tests. During the evaluation, healthcare professionals will assess the child's bladder and bowel habits, including the frequency and volume of urine output, the presence of any underlying medical conditions, and the child's overall health. In some cases, a voiding diary may be used to track the child's bladder and bowel patterns, providing valuable information for diagnosis and treatment planning.
It is important to note that elimination disorders are not a sign of poor parenting or a behavioral issue. They are medical conditions that require professional attention and management. Early diagnosis and intervention are crucial to helping children overcome these disorders and regain confidence in their bathroom habits. Treatment options may include behavioral therapies, such as bladder training and scheduled voiding, as well as the use of medications to address underlying medical issues that may contribute to the disorders.
Lenovo Tablets: Sleep and Wake Functionality Explored
You may want to see also

Psychological Factors: Emotional stress, anxiety, and trauma can contribute to the development of elimination disorders
Emotional stress, anxiety, and trauma play significant roles in the development and exacerbation of elimination disorders, which are a group of conditions characterized by the inability to control bowel movements or urination. These psychological factors can influence the body's physiological responses, leading to the physical symptoms associated with these disorders.
Stress is a well-known contributor to various health issues, and its impact on elimination disorders is no exception. When an individual experiences emotional stress, the body's stress response is triggered, leading to the release of stress hormones such as cortisol. These hormones can affect the digestive system, causing changes in bowel movements and potentially leading to incontinence. For example, stress-induced anxiety can cause muscle tension in the pelvic region, making it difficult to maintain control over bladder and bowel functions. This is particularly relevant for conditions like stress urinary incontinence and fecal incontinence.
Anxiety disorders are also closely linked to elimination disorders. Individuals with anxiety may experience heightened arousal and tension, which can directly impact the muscles involved in elimination. Panic attacks, a common symptom of anxiety disorders, can lead to sudden and intense symptoms, including urgency and incontinence. Moreover, anxiety can create a cycle of fear and avoidance, where individuals may develop a phobia of using the bathroom or experience severe anxiety around the possibility of accidents, further exacerbating the disorder.
Trauma, whether acute or chronic, can have profound effects on the mind and body. Traumatic events, such as accidents, abuse, or significant losses, can trigger the body's fight-or-flight response, which may result in the release of stress hormones and other physiological changes. In the context of elimination disorders, trauma can lead to the development of these conditions or cause existing symptoms to worsen. For instance, post-traumatic stress disorder (PTSD) is associated with increased risk factors for fecal incontinence, as individuals may experience severe anxiety and physiological reactions that interfere with normal bowel function.
Understanding the psychological factors at play is crucial in the management and treatment of elimination disorders. Therapies such as cognitive-behavioral therapy (CBT) can help individuals identify and manage stress, anxiety, and traumatic triggers. By addressing these emotional factors, patients can learn to cope with their disorders, improve their quality of life, and potentially reduce the physical symptoms associated with elimination disorders.
Mastering the Art of Waking a Deep Sleeper
You may want to see also

Treatment Approaches: Behavioral therapy, medication, and lifestyle changes are effective treatment options
Elimination disorders, characterized by the sudden and involuntary release of bodily waste in inappropriate places, can indeed be associated with sleep-wake disturbances, making it crucial to explore various treatment approaches. Behavioral therapy, a cornerstone of treatment, focuses on modifying the patient's behavior and addressing the underlying triggers. Therapists work closely with individuals to identify and understand the specific situations or emotions that prompt elimination behaviors. Through systematic desensitization and exposure therapy, patients are gradually exposed to anxiety-inducing situations, learning to manage their responses and reduce the frequency of eliminatory acts. Cognitive-behavioral therapy (CBT) is particularly effective, helping patients challenge and change negative thought patterns and behaviors.
In addition to behavioral interventions, medication can play a supportive role in managing elimination disorders. Selective serotonin reuptake inhibitors (SSRIs) and other antidepressants are commonly prescribed to help regulate mood and reduce anxiety, which can indirectly improve elimination behaviors. For severe cases, anti-anxiety medications may be recommended to provide immediate relief during particularly challenging periods. However, it is essential to note that medication should be used in conjunction with other treatment modalities for optimal results.
Lifestyle modifications are another crucial aspect of treatment. Encouraging regular bowel movements and bladder control through a consistent bathroom routine is essential. Patients are advised to maintain a healthy diet, stay hydrated, and avoid known triggers such as certain foods or stress factors. Adequate sleep hygiene practices are also vital, as sleep deprivation can exacerbate elimination behaviors. Establishing a relaxing bedtime routine and ensuring a comfortable sleep environment can significantly contribute to improving sleep quality.
Combining these treatment approaches can lead to significant improvements in managing elimination disorders and associated sleep-wake disturbances. Behavioral therapy provides patients with the tools to understand and manage their condition, while medication offers chemical support to alleviate symptoms. Lifestyle changes empower individuals to take control of their health, fostering a sense of independence and self-care. A comprehensive treatment plan, tailored to the patient's needs, can lead to long-term management and an improved quality of life.
Effective Strategies to Gently Awaken Deep Sleepers
You may want to see also

Prognosis and Management: With proper treatment, many individuals can achieve remission and improved sleep quality
The management and treatment of elimination disorders, a subset of sleep-wake disorders, often involve a comprehensive approach aimed at addressing the underlying causes and symptoms. With appropriate interventions, individuals can experience significant improvements in their sleep patterns and overall quality of life. Here's an overview of the prognosis and management strategies:
Prognosis:
Elimination disorders, such as nocturnal enuresis (bedwetting) and encopresis (soiling), are typically developmental issues that resolve over time. The prognosis is generally positive, especially when these disorders are identified early and managed effectively. Many children outgrow these conditions without any long-term consequences. However, if left untreated, these disorders can persist and impact a child's emotional well-being, self-esteem, and social interactions.
Management and Treatment:
- Behavioral Therapy: One of the primary management strategies is behavioral therapy, which focuses on modifying the child's behavior and addressing any associated psychological factors. Techniques may include bladder training, which involves teaching the child to recognize and control bladder sensations, and scheduled voiding, where the child is encouraged to use the toilet at regular intervals. For encopresis, therapy may include dietary adjustments, bowel training, and addressing any emotional or behavioral triggers.
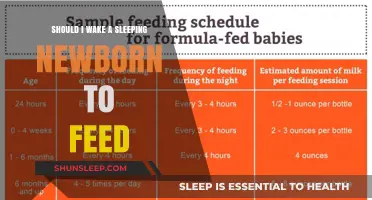
- Lifestyle Modifications: Implementing certain lifestyle changes can significantly contribute to managing elimination disorders. For bedwetting, this might include establishing a consistent bathroom routine, ensuring adequate fluid intake during the day, and limiting fluids before bedtime. In the case of encopresis, dietary modifications, such as increasing fiber intake and maintaining a regular bowel schedule, can be beneficial.
- Medications: In some cases, healthcare professionals may prescribe medications to manage specific symptoms. For instance, desmopressin acetate is a medication that can reduce the production of antidiuretic hormone, helping to control bedwetting episodes. For encopresis, medications may be used to manage severe constipation or other associated conditions.
- Psychological Support: Addressing the emotional impact of these disorders is crucial. Cognitive-behavioral therapy (CBT) can help children understand and manage their symptoms, improve their self-esteem, and develop coping strategies. Parental involvement and education are also essential, as they play a vital role in implementing treatment plans and providing ongoing support.
- Remission and Improved Sleep Quality: With proper treatment, many individuals can achieve remission, meaning they no longer experience the primary symptoms of elimination disorders. This often leads to improved sleep quality, as the underlying causes of sleep disturbances are addressed. Over time, the frequency and severity of episodes typically decrease, allowing individuals to regain a sense of normalcy and confidence in their ability to manage their condition.
In summary, elimination disorders are manageable conditions, and with the right approach, individuals can achieve remission and enjoy better sleep. Early intervention, a combination of behavioral and medical treatments, and ongoing support from healthcare professionals and families contribute to positive outcomes. It is essential to tailor the management plan to the specific needs of each individual, ensuring a holistic approach to care.
Understanding Sleep Talking: Why Waking Them Up Can Be Harmful
You may want to see also
Frequently asked questions
No, elimination disorders are not classified as sleep-wake disorders. Sleep-wake disorders, also known as sleep-wake disturbances or circadian rhythm disorders, primarily affect the timing and quality of sleep. They include conditions like insomnia, hypersomnia, narcolepsy, and delayed sleep phase disorder. Elimination disorders, on the other hand, are a group of conditions characterized by the inability to control the release of urine or feces, often associated with psychological stress or developmental issues.
While elimination disorders and sleep-wake disorders are distinct categories, there can be some overlap in symptoms and underlying causes. For example, children with bedwetting (nocturnal enuresis), a common elimination disorder, may experience sleep disturbances due to frequent awakenings or worry about accidents. Similarly, some sleep-wake disorders, like sleep apnea, can lead to daytime sleepiness and may impact a person's ability to control their bladder or bowel movements. However, these are not considered sleep-wake disorders themselves.
In some cases, yes. Certain sleep-wake disorders can contribute to the development or exacerbation of elimination disorders. For instance, individuals with insomnia or other sleep disturbances may experience increased stress, anxiety, or fatigue, which can lead to or worsen symptoms of bedwetting or encopresis (loss of bowel control). Addressing the sleep-wake disorder may help improve the management of elimination disorders and vice versa.