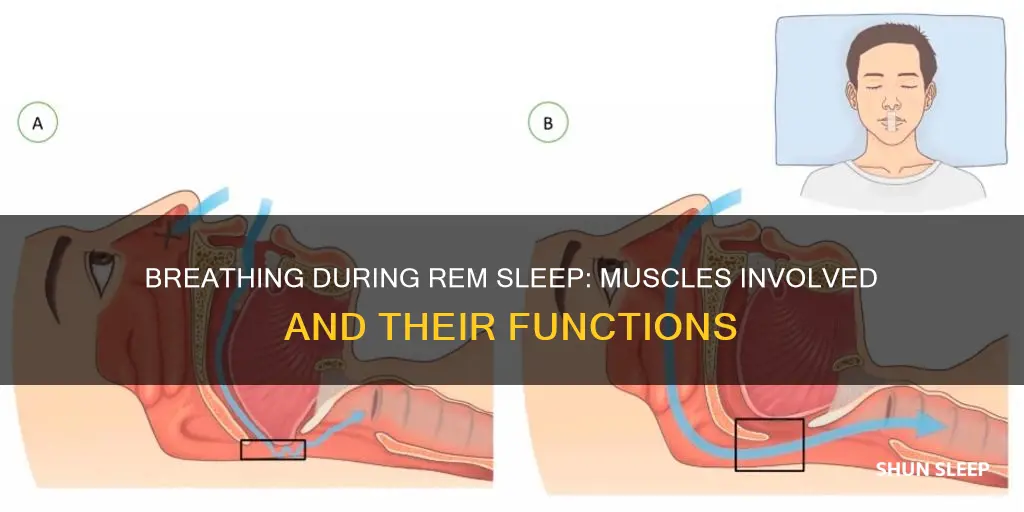
During sleep, the breathing rate goes up and down, and this is influenced by the stage of sleep. During non-REM sleep, breathing is slow and regular, but during REM sleep, the breathing rate increases, becoming faster and irregular. This is also the stage when we dream. Breathing becomes more shallow and less regular, possibly due to throat muscles relaxing and reduced movement of the rib cage. The diaphragm and accessory muscles are differently affected by sleep. Diaphragmatic function is largely preserved, but accessory muscle function is reduced, particularly during REM sleep.
| Characteristics | Values |
|---|---|
| Muscle activity | Intercostal muscle activity decreases, and the contribution of the rib cage to respiration decreases. |
| Diaphragm activity | Diaphragmatic activity increases during REM sleep. |
| Throat muscles | Throat muscles relax during REM sleep. |
What You'll Learn

Intercostal muscle activity decreases during REM sleep
During REM sleep, breathing becomes more shallow and irregular. This is due to the relaxation of the throat muscles and reduced movement of the rib cage. The intercostal muscles, which are located between the ribs, experience decreased activity during REM sleep. This reduction in intercostal muscle function leads to a decrease in the contribution of the rib cage to respiration.
The external intercostal muscles contract when taking a breath, causing the ribs to lift. Conversely, the internal intercostal muscles contract during a forced exhalation. Intercostal muscle strain can be caused by repetitive movements or injuries to the torso. Such strains are a common cause of musculoskeletal chest pain.
During sleep, the activity of the intercostal muscles and other skeletal muscles gradually decreases from wakefulness to non-REM sleep, and then to REM sleep. This reduction in muscle activity is more pronounced during REM sleep, resulting in a marked motor inhibition. The intercostal muscles are particularly susceptible to this inhibitory influence, leading to a decrease in their contribution to breathing during REM sleep.
The decrease in intercostal muscle activity during REM sleep is primarily responsible for hypoventilation in individuals with borderline pulmonary function. This reduction in muscle function, coupled with the atonia of the pharyngeal dilator muscles, contributes to upper airway resistance and increased respiratory instability.
HRV Analysis: Nokia HR for REM Sleep Tracking
You may want to see also

Diaphragm activity increases during REM sleep
During REM sleep, the diaphragm, the main inspiratory muscle, experiences increased activity. This is in contrast to the intercostal muscles, which show decreased activity during this sleep stage. While the diaphragm's activity is similar in REM sleep and active wakefulness, it is greater than in non-REM sleep. This increase in diaphragmatic activity during REM sleep may be due to an increase in central respiratory drive.
The increase in diaphragm activity during REM sleep is particularly notable in patients with unilateral diaphragm paralysis or severe weakness. These patients are at risk of developing sleep-disordered breathing during REM sleep, and their diaphragm electromyogram, reflecting neural respiratory drive, is doubled compared to healthy subjects, and further increased during REM sleep.
The diaphragm's activity during sleep is important for maintaining ventilation, and its function can be impacted by various factors such as body position and the presence of other respiratory abnormalities. For example, diaphragm paralysis may lead to breathlessness due to reduced respiratory system capacity.
Overall, the diaphragm plays a crucial role in breathing during REM sleep, and its activity during this sleep stage can have significant implications for respiratory health.
Dream Sleep: Understanding the REM Sleep Stage
You may want to see also

REM sleep is associated with irregular breathing
REM sleep is characterised by erratic breathing, with brief central apneas that can last from a few seconds to 20 seconds. This is in contrast to non-REM sleep, where breathing is slow and regular.
During REM sleep, the breathing pattern is affected by the behavioural system through REM sleep processes, fluctuating with ponto-geniculo-occipital (PGO) excitatory and inhibitory influences. The phasic phase of REM sleep is marked by bursts of PGO waves, which are thought to be linked to eye movements and irregular breathing.
The respiratory muscles are also affected by sleep state. There is a progressive fall in the activity of skeletal muscles with respiratory functions from wakefulness to NREM to REM sleep. The motor neurons are hyperpolarised during REM sleep, resulting in a marked motor inhibition.
The influence of sleep on respiratory muscles is not uniform. The upper airway dilator muscle activity demonstrates a progressive depression during the night, while the principal inspiratory muscles are relatively spared from the direct inhibitory influence of NREM sleep.
The intercostal muscle activity decreases during REM sleep, and the contribution of the rib cage to respiration also decreases. This decrease in intercostal muscle activity is responsible for the hypoventilation that occurs in patients with borderline pulmonary function.
The upper airway resistance is expected to be highest during REM sleep due to atonia of the pharyngeal dilator muscles and partial airway collapse. This can further decrease end-expiratory lung volume, reducing pharyngeal airway calibre and predisposing the upper airway to collapse.
The reasons for irregular breathing during REM sleep are not yet fully understood. However, studies have shown that it is likely due to a combination of factors, including the loss of the wakefulness stimulus, state-related fluctuations, and the reduction of respiratory muscle tone.
Enhancing REM Sleep: Tips for a Better Night's Rest
You may want to see also

Throat muscles relax during REM sleep
During REM sleep, the body experiences a range of changes, including fluctuations in breathing. While the breathing rate increases during REM sleep, it also becomes more shallow and irregular. This is due to a variety of factors, one of which is the relaxation of throat muscles.
During REM sleep, the throat muscles relax, which can contribute to a narrowing of the airway and a reduction in space for air to pass through. This relaxation of the throat muscles is one of the primary causes of snoring and can lead to a condition known as obstructive sleep apnea (OSA). OSA occurs when the airway becomes partially or completely blocked during sleep, resulting in disrupted breathing and reduced sleep quality. The condition is characterised by symptoms such as loud snoring, excessive daytime sleepiness, and morning headaches.
The relaxation of throat muscles during REM sleep is a normal biological process that affects both the respiratory and muscular systems. It is one of several factors that contribute to the changes in breathing patterns during sleep. In addition to the relaxation of throat muscles, there is also a decrease in movement of the rib cage during REM sleep, which further contributes to the irregular breathing patterns observed during this sleep stage.
While the relaxation of throat muscles during REM sleep is a natural and typical occurrence, it can have implications for individuals with certain risk factors. For example, people with specific anatomical features, such as a larger tongue or a shorter lower jaw, may be more prone to developing OSA due to the increased likelihood of airway obstruction. Additionally, factors such as age, sex, body weight, and sleeping position can also influence the development of OSA.
It is important to note that while OSA is a common sleep disorder, it can have serious health consequences if left untreated. Therefore, it is crucial to consult a doctor or sleep specialist if you suspect you may be at risk for OSA or are experiencing any symptoms of sleep-disordered breathing.
Trintellix and REM Sleep: What's the Connection?
You may want to see also

Upper airway dilator muscle function is compromised during REM sleep
During sleep, our breathing changes due to biological processes that affect our respiratory and muscular systems. One of the muscles responsible for breathing during REM sleep is the diaphragm, which experiences increased activity during this stage. However, upper airway dilator muscle function is compromised during REM sleep, which can lead to obstruction and conditions such as sleep apnea.
Upper airway dilator muscles, such as the genioglossus and tensor palatini, play a crucial role in maintaining upper airway patency. During REM sleep, the activity of these muscles decreases, leading to a reduction in airway collapsibility and an increase in airway resistance. This decrease in muscle activity is associated with a higher severity of obstructive sleep apnea during REM sleep compared to non-REM sleep. The reduction in muscle tone during REM sleep can be attributed to the loss of the wakefulness stimulus and the state-related fluctuation of excitatory and inhibitory impacts on respiration.
The loss of the wakefulness drive during sleep can have a significant impact on ventilatory control. In the absence of this stimulus, respiration becomes more sensitive to transient reductions in carbon dioxide levels and is more prone to apnea. Additionally, the reduced respiratory muscular tone during sleep, particularly during REM sleep, can exacerbate alveolar hypoventilation.
Furthermore, the state-related fluctuation of excitatory and inhibitory impacts on respiration also contributes to the compromised function of upper airway dilator muscles during REM sleep. The breathing pattern during REM sleep is influenced by the activation of the behavioral respiratory control system by REM sleep processes. This can lead to irregular breathing patterns, with sudden changes in amplitude and frequency.
In summary, upper airway dilator muscle function is indeed compromised during REM sleep due to various biological and physiological factors. This can have implications for respiratory health and conditions such as sleep apnea.
REM and Deep Sleep: What's the Difference?
You may want to see also
Frequently asked questions
Sleep has a notable impact on breathing, primarily through the withdrawal of the wakefulness stimulus, alteration of chemical/non-chemical responses, and reduction of muscle tone, lung volume, and metabolic rate.
REM sleep is characterised by irregular breathing, with a faster and more inconsistent breathing rate, increased heart rate and blood pressure, and temporary paralysis of the arm and leg muscles. Non-REM sleep, on the other hand, is marked by slow and regular breathing, with a decreased ventilation rate.
Sleep has a detrimental impact on respiratory muscle function. Upper airway dilator muscle function is compromised, especially during REM sleep, which can lead to obstruction. The diaphragm function is largely preserved to maintain adequate ventilation, but accessory muscle function is reduced during REM sleep, potentially affecting lung mechanics.