Coping with chronic obstructive pulmonary disease (COPD) can be challenging, and one of the most frustrating symptoms is when it disrupts your sleep. Waking up frequently during the night due to COPD can lead to fatigue, decreased productivity, and a decline in overall quality of life. Understanding the reasons behind these sleep disturbances and learning effective strategies to manage them can significantly improve your well-being. This paragraph aims to explore the impact of COPD on sleep patterns and provide insights into how individuals can navigate this common issue.
What You'll Learn
- Shortness of Breath: Waking up gasping for air, feeling breathless, and struggling to breathe deeply
- Chest Tightness: A heavy, squeezing sensation in the chest, making it hard to breathe comfortably
- Coughing Fits: Frequent, intense coughing episodes that disrupt sleep and cause discomfort
- Night Sweats: Excessive sweating during the night, often accompanied by a feeling of anxiety or discomfort
- Fatigue and Discomfort: Feeling exhausted and achy, making it challenging to fall back asleep

Shortness of Breath: Waking up gasping for air, feeling breathless, and struggling to breathe deeply
Shortness of breath is a common symptom of COPD (Chronic Obstructive Pulmonary Disease) and can be particularly distressing when it occurs during the night, disrupting sleep and causing sudden awakenings. When you have COPD, your airways become narrowed and inflamed, making it difficult to breathe. This condition can lead to a range of sleep-related issues, including waking up frequently due to shortness of breath.
If you find yourself gasping for air and feeling extremely breathless upon waking, it is essential to understand the underlying cause. COPD can cause the muscles around the airways to tighten, leading to a phenomenon known as bronchospasm. This constriction of the airways can result in a sudden increase in respiratory rate and a feeling of suffocation. As you lie down, the weight of your chest and abdomen can put pressure on the lungs, further exacerbating the shortness of breath.
During sleep, the body's natural airway clearance mechanisms may not function optimally, especially in individuals with COPD. Mucus production tends to increase at night, and the body's ability to clear it may be compromised. This excess mucus can block airways, leading to wheezing and gasping for air. Additionally, the position of your body during sleep can impact breathing. Lying flat may cause the tongue to block the airway, and the diaphragm's position can affect respiratory function.
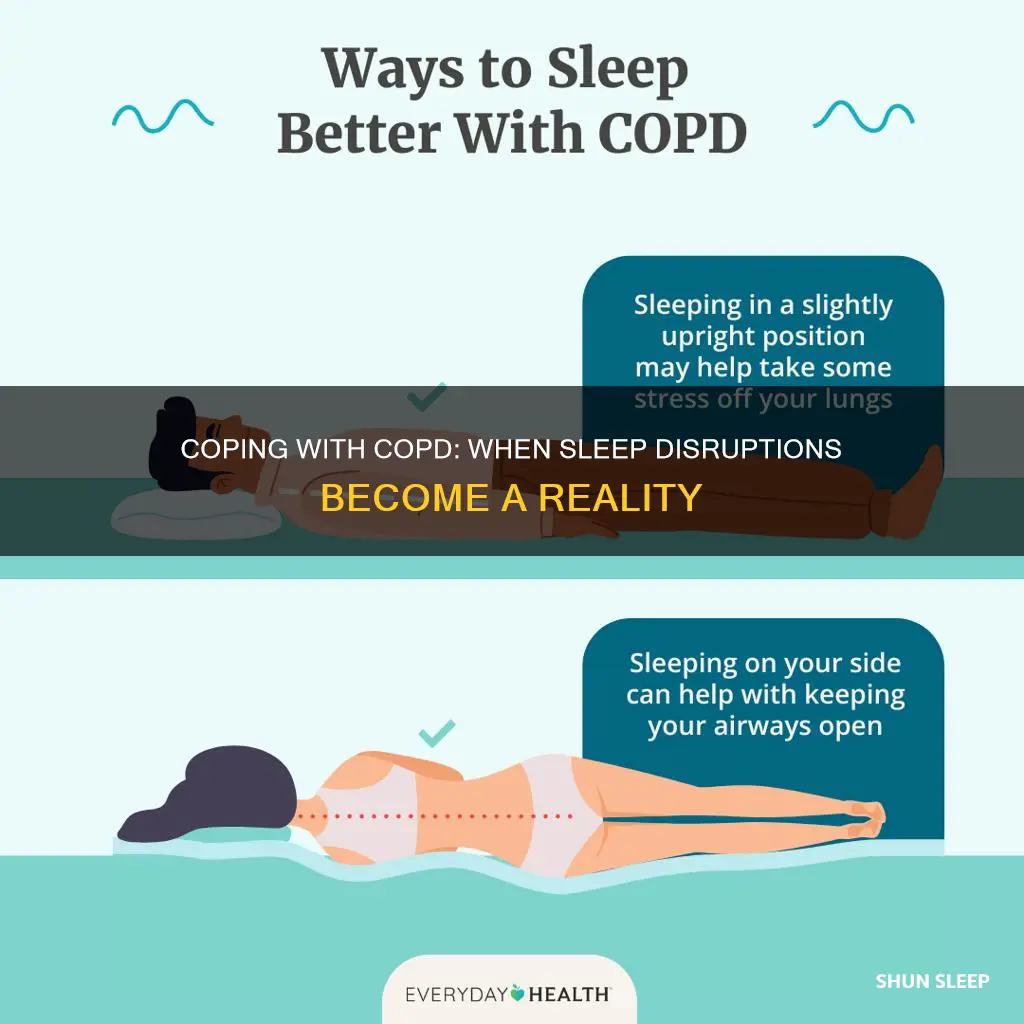
To manage this issue, it is crucial to establish a consistent sleep routine. Try to go to bed and wake up at the same time each day. Avoid lying flat; instead, sleep on your side or use extra pillows to elevate your head and open up the airways. Keep a humidifier running in your bedroom to add moisture to the air, which can help loosen mucus and reduce airway irritation. Regularly clear your airways by taking deep breaths and using a spirometer or peak flow meter to monitor your lung function.
If shortness of breath persists or worsens, it is imperative to seek medical attention. A healthcare professional can provide guidance on managing COPD symptoms and may recommend the use of bronchodilators or inhaled corticosteroids to help relax the airways and reduce inflammation. They may also suggest pulmonary rehabilitation programs, which can offer valuable education and support to improve breathing techniques and overall quality of life.
Troubleshooting: Windows 10 Computer Won't Wake from Sleep Mode
You may want to see also

Chest Tightness: A heavy, squeezing sensation in the chest, making it hard to breathe comfortably
Chest tightness is a common symptom experienced by individuals with chronic obstructive pulmonary disease (COPD), and it can significantly impact one's quality of life, especially when it disrupts sleep. When COPD patients wake up from sleep due to chest tightness, it often indicates an exacerbation or worsening of their condition. This symptom can be distressing and may lead to a cycle of anxiety and discomfort.
The sensation of chest tightness in COPD is often described as a heavy, squeezing pressure that makes breathing difficult. It can feel like someone is placing a tight band around the chest, making it hard to take deep breaths. This symptom is a result of the narrowing of airways and increased inflammation in the lungs, which are characteristic of COPD. When the airways constrict, they restrict airflow, leading to a feeling of suffocation and discomfort.
Waking up from sleep due to chest tightness can be a sign of several issues. Firstly, it may indicate that the individual's COPD is not well-managed, and their airways are becoming increasingly narrowed during the night. This can be a result of various factors, such as poor medication adherence, inadequate breathing support, or underlying sleep disorders like sleep apnea. Secondly, it could be a sign of an acute exacerbation of COPD, where the lungs suddenly become more inflamed and narrowed, leading to increased shortness of breath and chest tightness.
Managing chest tightness and its impact on sleep is crucial for COPD patients. Here are some strategies that can help:
- Medications: Ensure that prescribed medications, including bronchodilators and inhaled corticosteroids, are taken regularly. These medications can help relax the airways and reduce inflammation, providing relief from chest tightness.
- Breathing Exercises: Practicing deep breathing techniques can help open up the airways and improve oxygen flow. Techniques like diaphragmatic breathing or pursed-lip breathing can be particularly beneficial.
- Pulmonary Rehabilitation: Enrolling in a pulmonary rehabilitation program can offer comprehensive support. These programs often include education, exercise training, and strategies to manage symptoms, helping patients gain better control over their condition.
- Sleep Hygiene: Maintaining good sleep hygiene is essential. This includes creating a comfortable sleep environment, establishing a consistent sleep schedule, and avoiding triggers that worsen symptoms, such as smoking or exposure to irritants.
- Medical Assessment: Regular check-ups with a healthcare provider are vital. They can help monitor the condition, adjust treatment plans, and provide guidance on managing symptoms effectively.
In summary, chest tightness that disrupts sleep in COPD patients is a serious concern. It highlights the need for effective management strategies and close collaboration with healthcare professionals to ensure a better quality of life. By addressing the underlying causes and implementing appropriate interventions, individuals with COPD can find relief and improve their overall well-being.
The Ultimate Guide to Falling Asleep and Waking Up Restored
You may want to see also

Coughing Fits: Frequent, intense coughing episodes that disrupt sleep and cause discomfort
Coping with the symptoms of Chronic Obstructive Pulmonary Disease (COPD) can be challenging, especially when it disrupts your sleep. One of the most distressing and disruptive symptoms for many individuals with COPD is frequent and intense coughing fits. These episodes can not only cause discomfort but also lead to a cycle of sleep deprivation, which can further exacerbate the overall health and well-being of the individual.
During a coughing fit, the body's natural reflex to clear the airways can become exaggerated, leading to a series of rapid and forceful coughs. This can be particularly problematic at night when the body is in a relaxed state, making it harder to control the coughing reflex. The intense nature of these coughs often results in a sudden jolt from sleep, leaving individuals feeling exhausted and frustrated.
The impact of these coughing episodes on sleep quality is significant. Frequent awakenings can lead to a condition known as sleep fragmentation, where the sleep cycle is disrupted, and the individual struggles to achieve deep, restorative sleep. Over time, this can contribute to fatigue, decreased concentration, and a reduced quality of life. It is essential to understand the triggers and develop strategies to manage these coughing fits effectively.
Identifying the triggers for these intense coughing episodes is the first step towards finding relief. Common triggers include exposure to cold air, sudden changes in temperature, or even certain foods and drinks. For instance, a hot, spicy meal might initiate a coughing fit, while a cold, refreshing drink could provide temporary relief. Keeping a journal to track these triggers can be beneficial in tailoring a personalized approach to managing COPD symptoms.
In addition to recognizing triggers, individuals with COPD can employ various techniques to minimize the impact of coughing fits on their sleep. Simple measures such as maintaining a consistent sleep schedule, creating a comfortable sleep environment, and practicing relaxation techniques before bed can all contribute to better sleep quality. Furthermore, staying hydrated, avoiding known triggers, and using appropriate medications to manage symptoms can significantly reduce the frequency and intensity of these disruptive coughing episodes.
Fajr and Sleep: Navigating Early Risers' Schedules
You may want to see also

Night Sweats: Excessive sweating during the night, often accompanied by a feeling of anxiety or discomfort
Night sweats, characterized by excessive sweating during the night, can be a distressing symptom for individuals with Chronic Obstructive Pulmonary Disease (COPD). This condition, which encompasses emphysema and chronic bronchitis, often leads to sleep disturbances, and night sweats can exacerbate the discomfort and anxiety associated with COPD. Understanding the underlying causes and implementing appropriate management strategies are crucial for improving sleep quality and overall well-being.
One of the primary reasons COPD patients experience night sweats is the increased work of breathing. As COPD progresses, the lungs become less efficient at gas exchange, leading to hypoxemia (low oxygen levels in the blood). The body senses this oxygen deprivation and triggers a reflex that causes increased sweating as a mechanism to cool the body and improve oxygen absorption. This excessive sweating can occur during the night, disrupting sleep and causing discomfort.
Additionally, the underlying inflammation and increased metabolic rate associated with COPD can contribute to night sweats. Chronic inflammation in the body can lead to a heightened metabolic state, which may result in increased heat production and subsequent sweating. This is further exacerbated by the use of certain medications, such as bronchodilators and corticosteroids, which can have side effects that include night sweats.
Managing night sweats in COPD patients involves a multifaceted approach. Firstly, maintaining optimal room temperature is essential. A cool, well-ventilated bedroom environment can help reduce the feeling of overheating. Patients should also ensure they are wearing lightweight, breathable clothing to allow for better heat dissipation.
Furthermore, addressing the underlying COPD symptoms is crucial. This may include adhering to prescribed medications, such as inhaled bronchodilators and corticosteroids, to control inflammation and reduce the frequency of nocturnal awakenings. Pulmonary rehabilitation programs can also be beneficial, as they focus on improving lung function and overall exercise capacity, which can indirectly help manage night sweats.
In some cases, consulting a healthcare professional is necessary to rule out other potential causes of night sweats. Conditions like hyperthyroidism, certain medications, or even sleep apnea can contribute to excessive sweating during the night. Proper diagnosis and management of these underlying conditions can significantly improve the quality of life for COPD patients.
Revitalize Your Sleep: Tips to Wake Up Your Restful Haven
You may want to see also

Fatigue and Discomfort: Feeling exhausted and achy, making it challenging to fall back asleep
When individuals with COPD (Chronic Obstructive Pulmonary Disease) experience sleep disturbances, particularly waking up feeling exhausted and achy, it can significantly impact their overall quality of life. This fatigue and discomfort often create a challenging cycle, making it difficult to fall back asleep and leading to a lack of restorative sleep. Understanding the underlying causes and implementing effective strategies can help manage these symptoms and improve sleep patterns.
One of the primary reasons for fatigue and discomfort in COPD patients is the nature of the disease itself. COPD is characterized by chronic inflammation and narrowing of the airways, which can lead to increased breathlessness and shortness of breath during physical activities. When lying down, especially at night, these symptoms may intensify, causing patients to wake up frequently. The body's natural response to these physical discomforts can result in restlessness and an inability to find a comfortable position, leading to insomnia.
Additionally, the body's response to the underlying condition of COPD can contribute to fatigue. The chronic inflammation associated with COPD can trigger the release of inflammatory cytokines, which may affect the body's energy production and utilization. This can lead to a constant state of fatigue, even during periods of rest. Furthermore, the increased metabolic demand on the body due to respiratory issues can further exacerbate feelings of exhaustion.
To address these challenges, several strategies can be employed. Firstly, maintaining a consistent sleep schedule is crucial. Establishing a regular bedtime routine and ensuring adequate sleep hygiene practices can significantly improve sleep quality. This includes creating a comfortable sleep environment, minimizing noise and light disturbances, and using appropriate bedding and pillows to support the body.
Incorporating relaxation techniques before bedtime can also be beneficial. Deep breathing exercises, meditation, or gentle stretching can help calm the mind and body, reducing the physical and mental discomfort associated with COPD. Additionally, staying hydrated during the day and avoiding excessive fluid intake close to bedtime can minimize the need to urinate frequently during the night, which can disrupt sleep.
For those experiencing severe fatigue and discomfort, consulting a healthcare professional is essential. They may recommend specific medications or therapies to manage COPD symptoms, such as bronchodilators or inhaled corticosteroids. Additionally, referring patients to a sleep specialist can provide personalized advice and interventions to improve sleep patterns and overall well-being.
In summary, fatigue and discomfort caused by COPD can significantly impact sleep quality. By understanding the underlying causes and implementing practical strategies, individuals with COPD can take control of their sleep patterns and improve their overall health and quality of life. It is important to seek professional guidance to develop a comprehensive management plan tailored to individual needs.
Awakening Love: Strategies to Revive Your Sleeping Heart
You may want to see also
Frequently asked questions
COPD (Chronic Obstructive Pulmonary Disease) can disrupt sleep due to various factors. Firstly, the underlying condition often causes shortness of breath, leading to frequent awakenings as your body tries to regulate oxygen levels. Additionally, the need to clear mucus and the body's response to reduced oxygen saturation during sleep can further contribute to disrupted sleep patterns.
Managing COPD symptoms can significantly enhance sleep quality. Here are some tips:
- Establish a consistent sleep schedule and create a relaxing bedtime routine.
- Keep a humidifier in your bedroom to ease breathing and reduce nighttime awakenings.
- Practice deep breathing exercises or use a spirometer to help clear airways before bed.
- Avoid stimulants like caffeine close to bedtime, and limit alcohol intake as it can worsen breathing.
- Consider using oxygen therapy prescribed by your doctor to ensure adequate oxygen levels during sleep.
Yes, it is common for COPD patients to experience more coughing at night. This is often due to the body's natural rhythm and the effects of lying down, which can trigger mucus production and coughing fits. Using a humidifier and staying hydrated can help manage this symptom.
Yes, COPD can contribute to insomnia and other sleep disorders. The frequent awakenings and breathing difficulties can lead to difficulty falling back asleep, resulting in insomnia. Additionally, conditions like sleep apnea, where breathing temporarily stops during sleep, are more prevalent in COPD patients, further disrupting sleep patterns.
Gentle exercises can help improve sleep quality for COPD patients. Try light aerobic activities like walking, swimming, or cycling for 20-30 minutes daily. These exercises can strengthen your respiratory muscles, improve endurance, and promote better sleep. However, always consult your healthcare provider before starting any new exercise regimen.