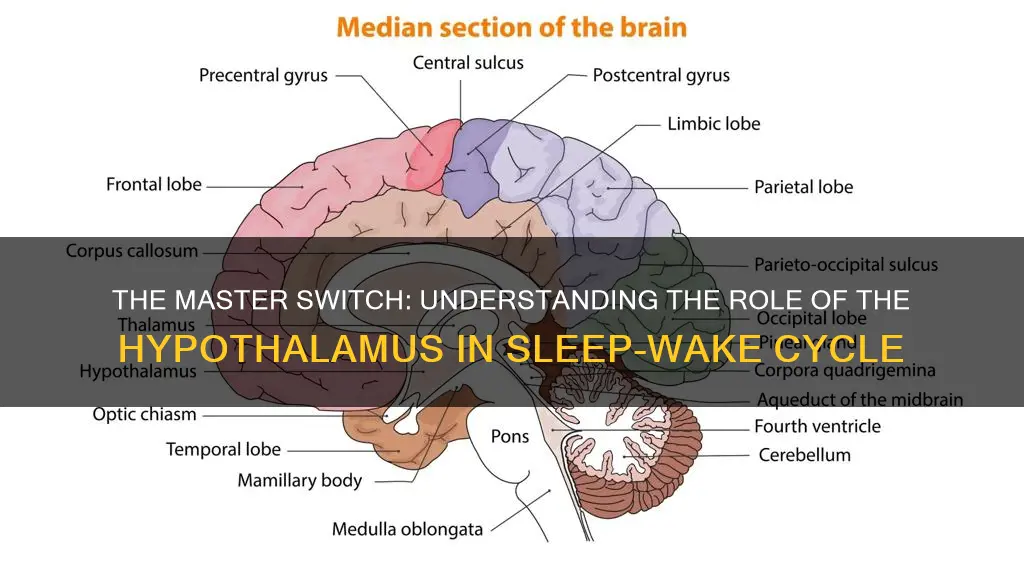
The regulation of sleep and wake cycles, or circadian rhythms, is a complex process involving multiple brain regions. Among these, the hypothalamus, a small but crucial part of the brain, plays a pivotal role in controlling sleep and wakefulness. Within the hypothalamus, the suprachiasmatic nucleus (SCN) is the master regulator of circadian rhythms. It receives light information from the eyes and coordinates the body's internal clock, influencing various physiological processes, including sleep, hormone release, and body temperature. Understanding the SCN's function provides valuable insights into the intricate mechanisms governing our daily cycles of rest and activity.
What You'll Learn
- Brain Regions Involved: The hypothalamus, specifically the suprachiasmatic nucleus, regulates sleep-wake cycles
- Neurotransmitters and Hormones: Melatonin and cortisol play key roles in sleep-wake rhythm
- Light Sensitivity: The retina's response to light influences circadian rhythm
- Genetic Factors: Certain genes, like PER2, influence sleep-wake timing
- Environmental Influences: Light exposure and temperature affect sleep-wake patterns

Brain Regions Involved: The hypothalamus, specifically the suprachiasmatic nucleus, regulates sleep-wake cycles
The human brain is an intricate network of regions, each with its unique functions and roles. When it comes to regulating our sleep-wake cycles, a specific area within the brain takes center stage: the hypothalamus, particularly its suprachiasmatic nucleus (SCN). This region is often referred to as the body's internal clock, orchestrating the complex dance between sleep and wakefulness.
The SCN is a small cluster of cells located in the hypothalamus, but its influence is far-reaching. It receives light information through the retina of the eyes, which is then transmitted to the SCN. This light input is crucial in synchronizing our internal clock with the external day-night cycle. As a result, the SCN helps to regulate the timing of various physiological processes, including body temperature, hormone release, and, most notably, sleep.
This brain region is highly sensitive to light, which is why exposure to natural sunlight during the day is essential for maintaining a healthy sleep-wake cycle. The SCN uses this light information to adjust the body's internal clock, ensuring that we feel alert during the day and ready for sleep at night. This process is often referred to as the circadian rhythm, a term derived from the Latin words for "about a day," emphasizing the daily cycles our bodies follow.
In addition to light cues, the SCN also integrates other signals to maintain the body's sleep-wake rhythm. For instance, it receives input from the brain's reticular activating system, which is involved in arousal and wakefulness. This integration of various signals allows the SCN to fine-tune our sleep patterns, ensuring we get the rest we need.
Understanding the role of the hypothalamus, especially the SCN, in sleep regulation has significant implications for various health conditions. For example, disruptions in this system can lead to sleep disorders, such as insomnia or delayed sleep phase syndrome. Moreover, this knowledge is valuable in developing strategies to improve sleep quality and overall well-being, highlighting the importance of this brain region in our daily lives.
Unveiling the Mystery: iPad's Wake and Sleep Sensor
You may want to see also

Neurotransmitters and Hormones: Melatonin and cortisol play key roles in sleep-wake rhythm
The sleep-wake cycle, also known as the circadian rhythm, is a complex process regulated by various neurotransmitters and hormones in the body. Among these, melatonin and cortisol are particularly crucial in maintaining the body's natural sleep-wake rhythm.
Melatonin, often referred to as the 'sleep hormone,' is primarily produced by the pineal gland, a small gland located in the brain. Its production is influenced by the body's internal clock, which is set by environmental cues, particularly light exposure. During the day, the pineal gland secretes minimal amounts of melatonin. However, as evening approaches and darkness falls, the pineal gland detects the absence of light and increases melatonin production. This increase in melatonin levels helps prepare the body for sleep by inducing drowsiness and promoting relaxation. Melatonin's role in regulating sleep is essential, as it helps synchronize the body's internal clock with the external environment, ensuring that we feel sleepy at night and alert during the day.
On the other hand, cortisol, often called the 'stress hormone,' is primarily produced by the adrenal glands, located on top of the kidneys. Cortisol levels follow a daily rhythm, typically peaking in the early morning, providing a surge of energy to start the day. As the day progresses, cortisol levels gradually decline, reaching their lowest point in the evening, which helps facilitate sleep. Cortisol's role in the sleep-wake cycle is twofold. Firstly, it helps maintain alertness and energy levels during the day, ensuring we stay awake and engaged. Secondly, as cortisol levels drop in the evening, it creates a physiological environment conducive to sleep by promoting muscle relaxation and reducing stress.
The interplay between melatonin and cortisol is essential for maintaining a healthy sleep-wake rhythm. As melatonin levels rise in the evening, it signals the body to prepare for sleep, and cortisol levels start to decrease, further promoting relaxation. This harmonious dance of hormones ensures that we can fall asleep easily and wake up feeling refreshed. Disruptions to this balance, such as those caused by irregular sleep patterns or certain medical conditions, can lead to sleep disorders and daytime fatigue.
Understanding the roles of melatonin and cortisol in the sleep-wake cycle can provide valuable insights into promoting better sleep hygiene. For instance, exposure to natural light during the day, especially in the morning, can help regulate the body's internal clock and promote healthy melatonin production. Additionally, managing stress levels and maintaining a consistent sleep schedule can positively impact cortisol levels, thereby improving overall sleep quality.
Awakening the Slumbering Speedster: Strategies for Sedgewich Success
You may want to see also

Light Sensitivity: The retina's response to light influences circadian rhythm
The human body's circadian rhythm, or internal clock, is a complex process that regulates various physiological functions, including sleep-wake cycles. One of the key factors influencing this rhythm is light sensitivity, particularly the response of the retina to different wavelengths of light. The retina, a light-sensitive tissue located at the back of the eye, plays a crucial role in detecting and interpreting visual information, but it also has a significant impact on our circadian rhythm.
When light enters the eye, it is detected by specialized cells called photoreceptors, which are primarily responsible for vision. However, these photoreceptors also contribute to the regulation of circadian rhythms. The two types of photoreceptors involved in this process are rods and cones. Rods are highly sensitive to light and are primarily responsible for night vision, while cones function best in well-lit conditions and are involved in color vision. Both types of photoreceptors contain a light-sensitive pigment called photopigment, which is activated by different wavelengths of light.
The photopigment in the retina, specifically in the specialized cells called intrinsically photosensitive retinal ganglion cells (ipRGCs), is particularly sensitive to light. These cells are unique because they directly respond to light without the need for the visual cortex's processing. When exposed to light, the ipRGCs transmit signals to the brain, specifically to the master circadian clock located in the hypothalamus. This clock then regulates various physiological processes, including the release of hormones that promote sleep or wakefulness.
The response of the retina to light is a critical mechanism in synchronizing our internal clock with the external environment. During the day, when exposed to natural light, the retina's photoreceptors are activated, sending signals to the brain that help maintain a state of alertness. This promotes a healthy circadian rhythm, ensuring that we feel awake and ready for the day's activities. Conversely, in the absence of light, especially during the night, the photoreceptors are less active, allowing the body to prepare for sleep.
In summary, light sensitivity, particularly the retina's response to different wavelengths, plays a vital role in regulating the circadian rhythm. The photoreceptors in the retina, especially the ipRGCs, detect light and transmit signals to the brain, influencing the sleep-wake cycle. Understanding this process can help explain why exposure to certain types of light at specific times of the day can impact our energy levels, mood, and overall health.
The Science of Waking Up: How Your Body Knows When to Rise
You may want to see also

Genetic Factors: Certain genes, like PER2, influence sleep-wake timing
The intricate dance of our sleep-wake cycles is orchestrated by a complex interplay of genetic and environmental factors. Among the myriad of genes that contribute to this rhythm, the PER2 gene stands out as a key player. PER2, a member of the PER (Period) gene family, is a crucial component of the circadian clock, our body's internal timekeeper. This gene encodes a protein that forms part of a complex molecular mechanism known as the circadian clock feedback loop. This loop regulates the expression of various genes, ensuring that our biological processes, including sleep and wakefulness, occur at the appropriate times.
Research has revealed that variations in the PER2 gene can significantly impact an individual's sleep-wake timing. Certain alleles of PER2 are associated with advanced sleep phase syndrome, a condition where individuals fall asleep earlier and wake up earlier than usual. This suggests that the PER2 gene's influence on circadian rhythm is not just theoretical but has tangible effects on real-world sleep patterns. For instance, individuals with a specific PER2 variant may naturally feel the need to go to bed earlier and wake up more refreshed, indicating a genetic predisposition towards an earlier sleep-wake cycle.
The PER2 gene's role in sleep-wake regulation is particularly intriguing because it is part of a larger network of genes that collectively govern circadian rhythms. These genes, including PER1, PER3, and CRY (Cryptochrome), form a feedback loop that oscillates with a period of approximately 24 hours. This loop helps synchronize our internal clocks with the external environment, ensuring that our sleep-wake cycles are in harmony with the day-night cycle. Mutations or variations in these genes can disrupt this delicate balance, leading to sleep disorders and other circadian rhythm disturbances.
Understanding the genetic underpinnings of sleep-wake timing has profound implications for various fields. For instance, in the field of medicine, identifying genetic markers associated with sleep disorders can lead to more personalized treatment approaches. Additionally, in the realm of chronobiology, studying genes like PER2 can provide insights into the evolutionary origins of circadian rhythms and their adaptation to different environments. This knowledge can also be applied in fields such as space exploration, where individuals face unique challenges in maintaining sleep-wake cycles in microgravity.
In conclusion, the PER2 gene is a prime example of how genetic factors can significantly influence our sleep-wake cycles. Its role in the circadian clock feedback loop highlights the intricate relationship between our genes and our biological rhythms. As research continues to unravel the complexities of these genetic influences, we gain valuable insights into the personalized nature of sleep and the potential for tailored interventions to improve sleep health and overall well-being.
Mastering Early Bird Hours: Tips for a Productive Morning Routine
You may want to see also

Environmental Influences: Light exposure and temperature affect sleep-wake patterns
The human body's sleep-wake cycle, also known as the circadian rhythm, is a complex process influenced by various internal and external factors. Among these, environmental factors play a significant role in regulating our sleep patterns. Light exposure and temperature are two critical environmental elements that can significantly impact our sleep-wake cycles.
Light exposure is one of the most powerful environmental cues that can influence our circadian rhythm. The human eye contains specialized cells called photoreceptors that detect light and send signals to the brain, specifically to the hypothalamus, which is a crucial part of the brain involved in regulating sleep. When light enters the eye, it triggers the release of a hormone called cortisol, often referred to as the 'awakeness hormone'. This hormone helps to promote alertness and wakefulness during the day. Conversely, in the evening, when it's dark, the absence of light exposure signals the body to produce another hormone, melatonin, which is often referred to as the 'sleep hormone'. Melatonin helps to induce sleepiness and prepares the body for rest.
The timing and duration of light exposure throughout the day can significantly impact the quality and timing of sleep. Exposure to bright light during the day, especially in the morning, helps to synchronize our internal clock with the external environment, making it easier to fall asleep at night. This is why maintaining a consistent sleep schedule and getting exposure to natural sunlight during the day can improve sleep quality. On the other hand, exposure to artificial light, especially the blue light emitted by electronic devices, in the evening can disrupt the production of melatonin, leading to delayed sleep onset and reduced sleep quality.
Temperature also plays a crucial role in regulating sleep-wake patterns. The body's core temperature naturally fluctuates throughout the day, typically reaching its peak during the day and dropping in the evening. This temperature rhythm is closely linked to the sleep-wake cycle. As the body's temperature rises, it promotes alertness and wakefulness. During the day, the body's temperature is maintained at a relatively stable level, allowing for optimal cognitive performance. However, as evening approaches, the body's temperature begins to drop, signaling the body to prepare for sleep. A cooler environment can enhance this process, making it easier to fall asleep.
Maintaining a comfortable room temperature is essential for optimal sleep. Research suggests that a slightly cooler environment, around 60-67°F (15.5-19.5°C), can improve sleep quality. A cool bedroom helps to slow down the body's core temperature, inducing a state of relaxation and preparing the body for sleep. Warmer temperatures, on the other hand, can disrupt sleep, as they may interfere with the body's natural temperature drop in the evening. It's also worth noting that individual preferences for temperature can vary, and finding the right balance that suits one's needs is essential for a good night's rest.
In summary, environmental factors, particularly light exposure and temperature, have a profound impact on our sleep-wake cycles. Understanding and manipulating these factors can help individuals optimize their sleep patterns, leading to improved overall health and well-being.
Awakening the Soul: Escaping the Slumber of Spiritual Sleep
You may want to see also
Frequently asked questions
The hypothalamus, a small region deep within the brain, plays a crucial role in controlling sleep and wakefulness. It contains clusters of neurons that act as the body's internal clock, regulating the timing of sleep and wake states.
The hypothalamus is involved in the regulation of sleep by producing and releasing hormones that promote sleepiness and wakefulness. For example, the hormone orexin (also known as hypocretin) is produced by a subset of neurons in the hypothalamus and is essential for maintaining wakefulness. Disruptions in orexin production can lead to sleep disorders.
Yes, while the hypothalamus is a key player, other brain structures contribute to sleep-wake cycles as well. The brainstem, for instance, contains the reticular activating system (RAS), which is responsible for maintaining a state of consciousness and alertness. The amygdala and hippocampus, part of the limbic system, also play roles in regulating sleep and emotional responses.
Absolutely. Sleep disorders often require a multidisciplinary approach to treatment. This may include behavioral therapies, such as sleep hygiene education and stimulus control, to improve sleep habits. In some cases, medications can help regulate sleep patterns. Cognitive-behavioral therapy for insomnia (CBT-I) is a highly effective non-pharmacological treatment that helps individuals manage sleep problems by identifying and changing negative thought patterns and behaviors.