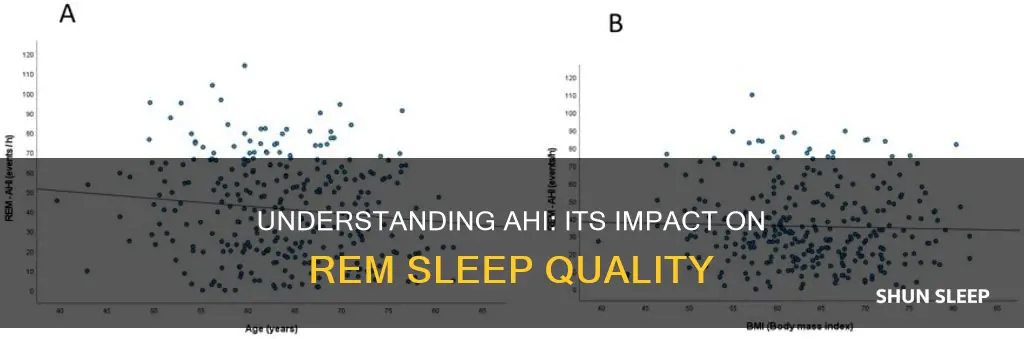
Obstructive sleep apnea (OSA) is a sleep disorder characterised by recurrent episodes of complete or partial collapse of the upper airway, which can occur during rapid eye movement (REM) sleep or non-rapid eye movement (NREM) sleep. The apnea-hypopnea index (AHI) is a diagnostic tool used to determine the presence and severity of OSA. It represents the average number of apneas and hypopneas (partial upper airway collapse) experienced each hour during sleep.
The AHI is calculated by dividing the total number of apneic and hypopneic events by the total number of hours of sleep. A normal AHI is less than 5 events per hour, while a severe AHI is more than 30 events per hour.
OSA during REM sleep is associated with distinct physiological alterations, including increased upper airway collapsibility, longer and more frequent apneas and hypopneas, and greater oxyhaemoglobin desaturation. It is also associated with marked hemodynamic variability, an increase in sympathetic activity, and greater myocardial demand.
OSA during REM sleep is a common disorder, with 10-37% of patients referred for OSA evaluation exhibiting apneas and hypopneas exclusively during this sleep stage. However, the health outcomes associated with OSA during REM sleep are not well understood. Some studies suggest that OSA during REM sleep is linked to objective sleepiness and impaired quality of life, while others have found no such associations. Recent evidence indicates that OSA during REM sleep may have cardiometabolic implications, including hypertension and alterations in glucose metabolism.
| Characteristics | Values |
|---|---|
| Definition | Apnea-Hypopnea Index (AHI) |
| Calculation | Average number of apneas and hypopneas per hour of sleep |
| Apnea | Complete collapse of the airway |
| Hypopnea | Partial collapse of the airway |
| Normal AHI | Less than 5 events per hour |
| Severe AHI | More than 30 events per hour |
| Diagnosis | Used to diagnose obstructive sleep apnea (OSA) |
| Polysomnography | Sleep study used to calculate AHI |
| ODI | Oxygen desaturation index |
What You'll Learn
- Apneas are periods when a person stops breathing, and hypopneas are instances when airflow is blocked, causing shallow breathing
- The AHI is calculated by dividing the number of apneas and hypopneas by the number of hours slept
- AHI scores for adults are divided into three categories: mild, moderate, and severe
- The AHI is different from the CAHI, which is used to diagnose central sleep apnea
- The AHI does not reveal how pauses in breathing affect blood oxygen levels

Apneas are periods when a person stops breathing, and hypopneas are instances when airflow is blocked, causing shallow breathing
Apneas and hypopneas are two breathing irregularities that occur during sleep. Obstructive sleep apnea (OSA) is a common sleep disorder that affects at least 2% to 4% of people. It is characterised by partial or complete obstructions of the airway during sleep, resulting in apneas and hypopneas. Apneas are periods when a person stops breathing, and hypopneas are instances when airflow is blocked, causing shallow breathing.
Apneas occur when a person's breathing completely stops or reduces to 10% of normal levels for at least 10 seconds. On the other hand, hypopneas occur when the airway partially collapses, resulting in shallow breathing. For an event to be considered a hypopnea, airflow must decrease by more than 30% for at least 10 seconds. Both apneas and hypopneas disrupt sleep, leading to lower blood oxygen levels and increasing the risk of long-term health complications.
The Apnea-Hypopnea Index (AHI) is a diagnostic tool used to determine the presence and severity of OSA. It represents the average number of apneas and hypopneas a person experiences each hour during sleep. AHI is calculated by dividing the total number of apneic and hypopneic events by the total number of hours of sleep. Normal AHI is less than 5 events per hour, while severe AHI is more than 30 events per hour.
While the AHI is a useful tool for diagnosing and assessing the severity of OSA, it has some limitations. For example, it does not take into account the duration of apneas and hypopneas, the impact on blood oxygen levels, or the pattern of breathing from hour to hour. Additionally, the definition of hypopneas can vary, leading to inconsistencies in AHI scores. Despite these drawbacks, the AHI is a valuable metric that guides healthcare professionals in their diagnosis and treatment decisions for OSA.
Fitbit's Sleep Tracking: Accurate or Just a Gimmick?
You may want to see also

The AHI is calculated by dividing the number of apneas and hypopneas by the number of hours slept
The apnea-hypopnea index (AHI) is a diagnostic tool for determining the presence and severity of obstructive sleep apnea (OSA). People with OSA experience a collapse of their airways during sleep. When this causes their breathing to completely stop or reduce to 10% of normal levels for at least 10 seconds, it is called an apnea. Hypopneas occur when your airways partially collapse, resulting in shallow breathing. If your airflow decreases by more than 30% for at least 10 seconds, it can be considered a hypopnea. Apneic and hypopneic events disrupt sleep and lead to lower blood oxygen levels, contributing to long-term health complications.
The AHI is calculated by dividing the total number of apneic and hypopneic events by the total number of hours slept. To register as an event, an apnea or hypopnea must last at least 10 seconds or longer. Doctors typically calculate AHI during a sleep study, or polysomnogram, which monitors your brain waves, blood oxygen levels, heart rate, and breathing while you sleep. While the AHI is the primary measurement for diagnosing OSA, your doctor may review other metrics to better understand the severity of your OSA.
The AHI is measured on a numeric scale. Scores for adults are divided into three categories, which correspond to different levels of OSA severity:
- Mild: An AHI of at least five events per hour, but fewer than 15.
- Moderate: An AHI of at least 15 events per hour, but fewer than 30.
- Severe: An AHI of at least 30 events per hour.
While five is the cutoff for adults, an AHI of one or above is sufficient to diagnose obstructive sleep apnea in children. Children breathe faster than adults in order to support their faster metabolism and smaller lung capacity. This is why even one apneic event can have more of an impact for a child.
Measuring REM Sleep: Jawbone's Unique Approach
You may want to see also

AHI scores for adults are divided into three categories: mild, moderate, and severe
The apnea-hypopnea index (AHI) is a diagnostic tool that helps determine the presence and severity of obstructive sleep apnea (OSA). It is the average number of apneas and hypopneas (partial or complete obstructions of the airway) experienced each hour during sleep. Apneas and hypopneas must last for at least 10 seconds to be counted.
- Mild: An AHI of at least five events per hour, but fewer than 15.
- Moderate: An AHI of at least 15 events per hour, but fewer than 30.
- Severe: An AHI of at least 30 events per hour.
An AHI of less than five events per hour is considered normal, while a score of 30 or more events per hour is classified as severe sleep apnea.
REM Sleep: Is Brief Enough for Health?
You may want to see also

The AHI is different from the CAHI, which is used to diagnose central sleep apnea
The Apnea-Hypopnea Index (AHI) is a diagnostic tool used to determine the presence and severity of Obstructive Sleep Apnea (OSA). It quantifies the severity of sleep apnea by counting the number of apneas (periods when a person stops breathing) and hypopneas (instances when the airflow is blocked, causing shallow breathing) during sleep. The AHI is calculated by dividing the total number of apneic and hypopneic events by the total number of hours of sleep. A normal AHI is less than 5 events per hour, while a severe AHI is more than 30 events per hour.
Now, it's important to note that the AHI is different from the Central Apnea-Central Hypopnea Index (CAHI), which is used specifically for diagnosing central sleep apnea. Central sleep apnea is a form of sleep apnea that occurs when the brain fails to signal the respiratory muscles to breathe. In contrast, OSA is caused by a collapse of the airways during sleep.
The distinction between AHI and CAHI is crucial because they refer to different types of sleep apnea with distinct underlying causes. While OSA is characterized by a collapse of the airways, central sleep apnea is a result of the brain's failure to signal the respiratory muscles to breathe. This differentiation is essential for accurate diagnosis and treatment.
Additionally, the AHI has some drawbacks. It does not take into account all factors that may indicate the severity of OSA. For example, it does not measure how long an apnea or hypopnea lasts, only that it occurs for at least 10 seconds. It also does not reveal how these breathing pauses affect blood oxygen levels, which is an important consideration for understanding the long-term health complications associated with sleep apnea.
In summary, while the AHI is a valuable tool for diagnosing and assessing the severity of OSA, it should be interpreted alongside other metrics and considerations for a comprehensive understanding of an individual's sleep apnea.
Understanding REM Sleep Cycles and Their Importance
You may want to see also

The AHI does not reveal how pauses in breathing affect blood oxygen levels
The Apnea-Hypopnea Index (AHI) is a diagnostic tool used to determine the presence and severity of Obstructive Sleep Apnea (OSA). It calculates the average number of apneas and hypopneas per hour during sleep. Apneas are periods when a person stops breathing, while hypopneas are instances where airflow is blocked, causing shallow breathing.
However, the AHI does not reveal how pauses in breathing affect blood oxygen levels. This is because the AHI only measures the number of respiratory events and does not show how these events affect blood oxygen levels. It also does not account for the duration of each event, only that it lasts at least 10 seconds. As a result, the AHI may not accurately reflect the severity of OSA and its potential health consequences.
Other factors that may be considered in addition to the AHI include the duration of apneas and hypopneas, blood oxygen levels, and patterns in breathing from hour to hour. These additional factors can provide a more comprehensive understanding of the impact of OSA on an individual's health.
It is important for healthcare professionals to consider multiple factors when diagnosing and treating OSA to ensure effective management of the condition.
Record REM Sleep: Tips for Capturing Your Dreams
You may want to see also
Frequently asked questions
AHI stands for apnea-hypopnea index. It is a diagnostic tool for determining the presence and severity of obstructive sleep apnea (OSA).
The AHI represents the average number of apneas and hypopneas a person experiences each hour during sleep. To measure it, doctors divide the total number of apneic and hypopneic events by the total number of hours the person was asleep.
A normal AHI is less than 5 events per hour, while severe AHI is more than 30 events per hour.
Obstructive sleep apnea during REM sleep is a common disorder. People with OSA experience a collapse of their airways during sleep. When this occurs during REM sleep, it is called REM-related OSA.