Sleep is a complex and mysterious body process that is vital for our health and well-being. During sleep, the body cycles through various stages, including non-REM sleep stages 1 to 4 and REM sleep. Each stage is associated with unique physiological changes and functions, and understanding these stages can provide insights into the role of sleep in regulating hormone levels. This paragraph serves as an introduction to the topic of hormone level changes during non-REM sleep stages 1 to 4, which will be explored in subsequent paragraphs.
What You'll Learn

Estrogen and progesterone levels
Estrogen and progesterone are the two major female hormones. Estrogen, the main female sex hormone, helps control the monthly menstruation cycle. Progesterone, its cousin, is the hormone that helps maintain pregnancy. It is known as the "relaxing hormone" and has a mildly sedative effect.
These two hormones shift up and down throughout a woman's life, affecting sleep along the way. For example, in the week before a woman's period, her progesterone levels will rise to prepare her body for a potential pregnancy. If there is no pregnancy, progesterone levels decrease dramatically, causing the uterine lining to shed and starting the menstrual cycle. Immediately before bleeding begins, a woman's progesterone levels dip dramatically, which is why some women can find it difficult to get quality sleep in the days leading up to their period. After menstruation, progesterone levels will slowly rise again, allowing for more restful sleep.
During pregnancy, both progesterone and estrogen levels increase significantly in the first trimester, which may be why many women report feeling drowsy and taking more naps during this time. By the third trimester, these hormone levels even out, but other factors such as frequent urination, restless leg syndrome, and difficulty breathing can make it challenging to get a good night's sleep.
As a woman approaches menopause, her hormone levels fluctuate dramatically, causing night sweats and hot flashes that can disrupt sleep. Additionally, lower levels of progesterone can make some women more irritable and less able to relax. Research suggests that progesterone and estrogen may protect women against sleep apnea, but this benefit is lost after menopause. Older women are just as likely to develop sleep apnea as men, and other sleep disorders also become more common.
During menopause, the decline in estrogen and progesterone levels can lead to sleep disturbances. Hormone replacement therapy has been shown to improve sleep quality during this time, indicating a positive relationship between estrogen and sleep in perimenopausal women. However, the association between endogenous estrogen and sleep is less clear in premenopausal women.
Progesterone generally has a sleep-promoting effect. A steep decline in progesterone during the late luteal phase of the menstrual cycle is associated with sleep disruption. Women tend to experience poorer sleep during this phase, reporting more wakefulness and arousals. Additionally, low levels of progesterone are associated with sleep-disordered breathing.
Muscle Activity in REM Sleep: What's Happening?
You may want to see also

Cortisol levels
Cortisol is a hormone produced by the hypothalamic pituitary adrenal (HPA) axis, which includes the hypothalamus and pituitary gland in the brain, as well as the adrenal glands, which sit on top of the kidneys. The HPA axis is responsible for coordinating our sleep cycles and when it is disrupted through poor nutrition, chronic stress, or illness, it can result in insomnia and other sleep disturbances.
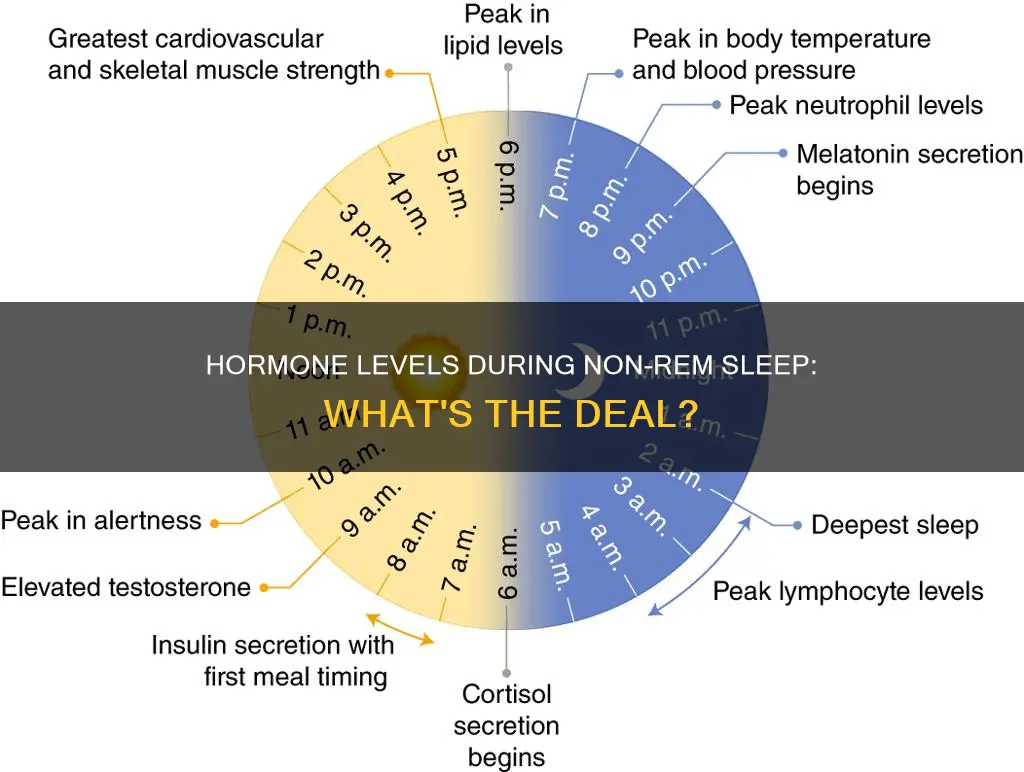
Cortisol production follows a 24-hour circadian rhythm, with levels dropping to their lowest point around midnight and peaking about an hour after waking up, typically around 9 a.m. This circadian cycle is complemented by 15 to 18 smaller pulses of cortisol released throughout the day and night, some of which correspond to shifts in our sleep cycles.
During non-REM sleep, our body goes through three stages. In the first stage, we transition from being awake to being asleep, which usually lasts a few minutes. In the second stage, our body temperature drops, and our breathing and heart rate continue to slow. The third stage is the deepest period of sleep, during which our heart rate, breathing, and brainwaves are at their slowest.
Studies have found that when the HPA axis is overly active, it can disrupt our sleep cycles, resulting in shortened overall sleep time and increased sleep disturbances. Sleep deprivation and insomnia can further disrupt the HPA axis, leading to distorted cortisol production. Chronic stress and traumatic experiences can also impact cortisol levels, with some research indicating that trauma survivors may have persistently elevated or decreased cortisol levels as a result of their HPA axis being constantly triggered.
Elevated cortisol levels have been associated with metabolic changes, including increased glucose and insulin levels, decreased adiponectin levels, and alterations in leptin and ghrelin levels, which can impact food intake and energy balance. Additionally, sleep deprivation has been linked to increased cortisol levels, reflecting impairment of HPA axis regulation and resulting in glucocorticoid overload, which can have deleterious effects on the body.
To lower cortisol levels and improve sleep, it is recommended to modify one's diet, take supplements like fish oil and ashwagandha, exercise regularly, practice mindfulness and meditation, and consider therapy with a trained mental health professional.
REM Sleep: Deep Sleep's Role in Brain Function
You may want to see also

Insulin, leptin, and ghrelin levels
Insulin is a storage hormone produced by the pancreas. It transfers glucose from food into your cells for energy or storage, depending on your body's needs. Insulin resistance occurs when cells stop responding to insulin, resulting in high blood sugar. This can lead to obesity, type 2 diabetes, and heart disease. To improve insulin sensitivity, it is recommended to exercise regularly, improve sleep habits, consume more omega-3 fatty acids, follow a Mediterranean diet, and maintain a moderate weight.
Leptin is a fullness hormone that signals to the hypothalamus when you are full. However, leptin resistance can occur in people with obesity, leading to overeating. To improve leptin levels, it is important to maintain a healthy weight, improve sleep quality, and exercise regularly.
Ghrelin is the hunger hormone that signals to the hypothalamus when your stomach is empty. It increases appetite, and its levels are typically highest before eating and lowest after a meal. Poor sleep and obesity can lead to increased ghrelin levels, resulting in overeating and weight gain. To manage ghrelin levels, it is recommended to maintain a moderate body weight, get good quality sleep, and eat regularly.
REM Sleep: The Body's Natural Healer?
You may want to see also

Human growth hormone levels
Human growth hormone (HGH) is released during the third stage of non-REM sleep, which is the final stage of non-REM sleep and the deepest period of sleep. This stage is marked by slow brain waves as the brain enters a deeper state of sleep compared to the first two stages of non-REM sleep. During this stage, the heartbeat and breathing slow to their lowest levels, and the muscles are so relaxed that a person may be difficult to awaken.
The amount of HGH released during sleep is directly related to the amount of slow-wave sleep a person gets. In adults, the most significant pulse of HGH secretion occurs shortly after falling asleep, during the first phase of slow-wave sleep. In men, around 70% of the HGH pulses during sleep coincide with slow-wave sleep, and the amount of HGH secreted during these pulses is correlated with the amount of slow-wave sleep.
Sleep-related HGH secretion appears to be primarily dependent on the release of growth hormone-releasing hormone. Studies in rodents and humans have shown that injections of growth hormone-releasing hormone decrease wakefulness and increase slow-wave sleep. During the third and fourth decades of life (ages 20 to 40), the total amount of HGH secreted over a 24-hour period decreases by two to three times. Similarly, the amount of slow-wave sleep decreases significantly over the same age range.
While sleep onset facilitates the release of HGH, the timing of other sleep stages, such as REM sleep, may alter the magnitude of sleep-related HGH secretion. For example, during REM sleep, which is a much deeper sleep than the non-REM sleep stages, there is increased brain activity, and the body is temporarily paralysed.
The Mystery of Missing REM Sleep: What's Keeping Me Awake?
You may want to see also

Melatonin levels
Melatonin is a hormone that plays a crucial role in regulating sleep-wake cycles. It is controlled by the body's internal clock, known as the circadian rhythm, which operates on a 24-hour cycle. This internal clock is located in the suprachiasmatic nucleus (SCN) of the hypothalamus. The SCN receives information about incoming light from the eyes and adjusts melatonin production accordingly.
When there is less light, such as during the night, the SCN signals the brain to increase melatonin production, making you feel sleepy. As your body prepares for sleep, you transition through the non-REM sleep stages, which consist of N1, N2, and N3. During these stages, your heart rate and breathing slow down, your body temperature drops, and your muscles relax.
In the final stage of non-REM sleep, N3, you enter into deep sleep. This is the stage when your body repairs and regenerates tissues, builds bone and muscle, and strengthens your immune system. It is also during this stage that human growth hormone (HGH) is released, aiding in the restoration and rebuilding of your body.
Throughout the night, your body cycles between non-REM and REM sleep. During REM sleep, your brain activity increases, and this is typically when dreams occur. The cycling between non-REM and REM sleep repeats approximately four to six times each night, with each cycle lasting around 90 to 120 minutes.
While melatonin levels are not directly mentioned for each stage of non-REM sleep, it is clear that melatonin plays a crucial role in the onset of sleep and in regulating sleep-wake cycles. Melatonin levels increase when it is dark, signalling to your body that it is time to prepare for sleep. As you progress through the non-REM sleep stages, your body gradually relaxes and slows down, reaching its lowest levels of activity during the deep sleep of the N3 stage.
Additionally, it is important to note that melatonin supplements are often used to aid sleep. While available over the counter, it is recommended to consult a healthcare provider before taking melatonin, especially for individuals over the age of 65.
The Importance of REM Sleep and How Much We Need
You may want to see also
Frequently asked questions
Non-REM sleep is important for regulating hormone levels, particularly those related to stress and hunger. During non-REM sleep, the body slows down, and this helps to balance hormone levels and prepare the body for the next day.
Many hormones are influenced by non-REM sleep, including melatonin, human growth hormone, cortisol, insulin, leptin, and ghrelin.
During non-REM sleep, the body produces and releases hormones that regulate various functions, such as metabolism, appetite, and sexual function. Non-REM sleep also helps to balance hormone levels by slowing down bodily functions and allowing the body to rest and recover.
Not getting enough non-REM sleep can lead to hormone imbalances, which can have negative effects on the body. This can include increased stress levels, weight gain, and a higher risk of illness or infection.