Sleep and depression are closely linked. While it is normal to enjoy sleeping in, if you find yourself struggling to get out of bed or get ready in the morning, this could be a sign of depression. Depression can make you feel physically and mentally fatigued, to the point where even small tasks can feel exhausting or difficult. This can lead to sleeping throughout the day, using sleep to pass the time, or choosing sleep over other daily activities. This condition is called hypersomnia, the opposite of insomnia.
Excessive sleeping is a common symptom of major depressive disorder. It may be a means of self-managing depression and escaping emotional pain. However, it is important to distinguish between fatigue, sleepiness, and depression. While all three issues can benefit from getting seven to eight hours of sleep per night, depression is marked chiefly by a low mood and loss of interest in pleasure for most days over a two-week period.
| Characteristics | Values |
|---|---|
| Excessive sleeping | A symptom of major depressive disorder |
| A way to escape emotional pain | |
| A physiological effect of the reduction of neurotransmitters | |
| A symptom of premenstrual dysphoric disorder | |
| A symptom of seasonal affective disorder | |
| A symptom of bipolar disorder |
What You'll Learn

Depression and insomnia often go hand-in-hand
Depression and insomnia often go hand in hand. Sleep issues are commonly associated with depression, and insomnia is one of the most prevalent. It is believed that about 15% of people with depression have hypersomnia or experience excessive daytime sleepiness.
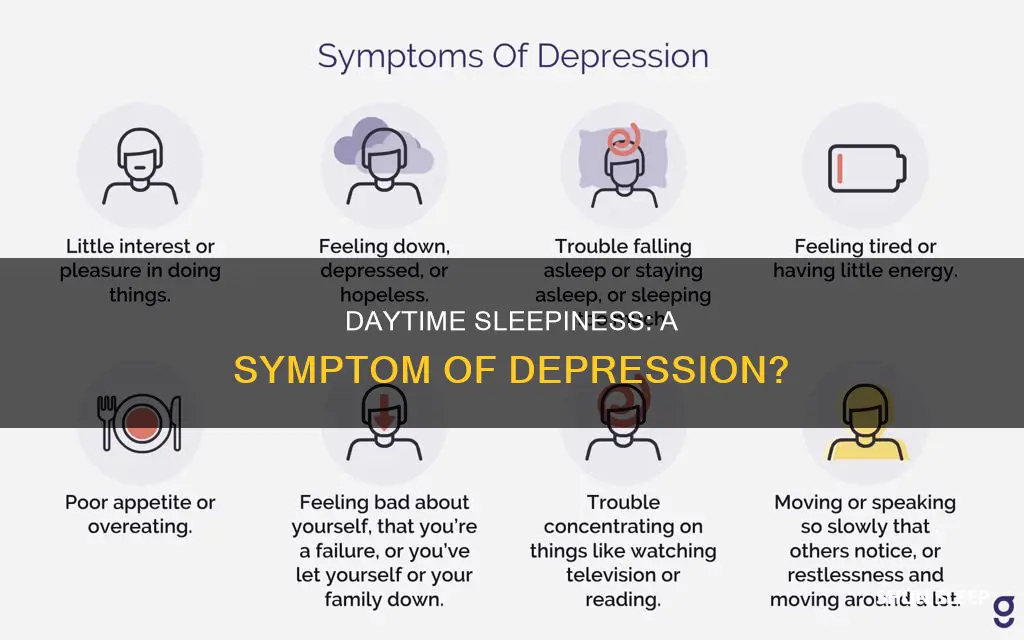
Depression is marked by persistent bouts of sadness, disappointment, and hopelessness, as well as other emotional, mental, and physical changes that lead to difficulties with daily activities. When difficult emotions remain present for more than two weeks, are felt nearly every day, and remain present for most of the day, they may be related to a group of mood disorders called depressive disorders.
Depression can make it difficult to fall asleep and stay asleep during the night. It can also cause periods of excessive daytime sleepiness. This can create a cycle where anxious thoughts keep one awake, leading to more anxious thoughts due to lack of sleep.
Depression and insomnia have a bidirectional relationship. Poor sleep can contribute to the development of depression, and having depression makes a person more likely to experience sleep troubles. This complex relationship can make it challenging to determine which came first, the sleep issues or the depression.
If you suspect that you or someone you know may be experiencing symptoms of depression, it is important to seek professional help.
The Real Reason Men Sleep With Women They Don't Love
You may want to see also

Excessive sleeping is a symptom of major depressive disorder
Excessive sleeping, or hypersomnia, is a common symptom of major depressive disorder. When people are feeling low, sleeping becomes an opportunity for relief. Depression can make people feel fatigued, both physically and mentally, and this can manifest as a desire to sleep for longer than usual.
The relationship between sleep and depression
The relationship between sleep and depression is bidirectional. This means that poor sleep can contribute to the development of depression, and having depression makes a person more likely to experience sleep troubles. For example, people with depression often experience insomnia, hypersomnia, or obstructive sleep apnea.
The impact of excessive sleeping
Excessive sleeping can have a negative impact on people's lives, affecting their careers, job security, relationships, and overall well-being. It can also disrupt family dynamics, especially when a parent is unable to care for their children due to their excessive sleeping.
Seeking help
When symptoms of depression, such as hypersomnia, are significantly impacting a person's quality of life, it is important to seek professional help. Depression is a serious mental health condition that can lead to daily impairments in all areas of life. Treatment for depression typically involves a combination of medication and psychotherapy.
The Mystery of My Nocturnal Habits Explained
You may want to see also

Depression can cause fragmented sleep
The relationship between sleep disturbances and depression is bidirectional, meaning that sleep problems can both result from and contribute to depression. Sleep disturbances in depressed individuals may be related to alterations in the regulation of sleep and wakefulness, such as changes in the circadian rhythm and disruptions in specific sleep stages, including REM sleep and slow-wave sleep. These changes can lead to decreased sleep quality, increased sleep fragmentation, and a higher risk of developing depression.
Additionally, the psychological mechanisms underlying sleep disturbances can further exacerbate depression. For example, individuals prone to insomnia and depression may hold more extreme or black-and-white beliefs, leading to a sense of hopelessness and a vicious cycle of agitation and sleep disturbance.
Addressing sleep disturbances is crucial in the treatment of depression. Cognitive-behavioral therapy for insomnia (CBT-I) has been found to be effective in treating insomnia and improving depression outcomes. Pharmacological interventions, such as hypnotics, sedating agents, and antidepressants, can also be used to manage sleep disturbances in depressed individuals. However, it is important to carefully select and monitor these medications due to potential side effects and interactions.
Puppy Sleep Patterns: What's Normal for New Adoptees?
You may want to see also

Sleep issues may influence the function of the neurotransmitter serotonin
Sleeping all day can be a sign of depression. Depression can often lead to sleeping more and a delayed sleep pattern, where an individual stays up later and sleeps later. This delayed sleep pattern can, in turn, worsen depression.
Now, onto serotonin. Serotonin is a chemical that carries messages between nerve cells in the brain and throughout the body. It is also a hormone. As a neurotransmitter, serotonin carries messages between nerve cells in the brain (the central nervous system) and throughout the body (the peripheral nervous system). These messages tell the body how to work.
Serotonin plays a role in many bodily functions, including mood, learning, memory, happiness, regulating body temperature, sleep, sexual behaviour, and hunger. A lack of serotonin is thought to play a role in depression, anxiety, mania, and other health conditions.
Serotonin, along with the neurotransmitter dopamine, plays a role in the quality of sleep. The brain needs serotonin to make melatonin, a hormone that regulates the sleep-wake cycle.
Firstly, serotonin is one of the chemicals that trigger sleep/wake cycles. Nerve cells in the brainstem release serotonin, which acts on parts of the brain to keep it alert and functioning while an individual is awake. When an individual is awake, the release of serotonin during this time leads to homeostatic regulation of slow-wave sleep. The longer one is awake, the greater the body senses the need to sleep.
Secondly, serotonin is produced in the body from the essential amino acid tryptophan, which must be obtained from food. Eating foods high in tryptophan will not necessarily boost serotonin levels on its own, as it is a complex process. The body needs carbohydrates to release insulin, which is needed to absorb amino acids. Then, even if tryptophan enters the bloodstream, it has to compete with other amino acids to be absorbed into the brain.
Thirdly, abnormal serotonin function can lead to insomnia. Experiments have shown that the destruction of serotonin neurons in the raphe system or the inhibition of serotonin synthesis results in severe insomnia. However, electrical activity in serotonin neurons and the release of serotonin increase during waking and decrease during sleep, which contradicts the hypothesis that serotonin is a true neuromodulator of sleep.
Finally, serotonin has been shown to control the synthesis of vasoactive intestinal peptide (VIP) in the suprachiasmatic nucleus (SCN). The SCN is an area of the brain that controls the body's internal clock and is sensitive to signals of dark and light. The release of melatonin, which makes an individual feel sleepy and ready for bed, is triggered when the SCN sends messages to the pineal gland during periods of darkness.
Staying Awake and Hungry: The Don't Eat, Don't Sleep Challenge
You may want to see also

Depression is a manageable mental health disorder
Depression is a serious mental health condition that can significantly impact a person's quality of life. It is the second most common mental health disorder experienced by Americans, affecting over 17 million people each year. It is characterised by persistent bouts of sadness, disappointment, and hopelessness, as well as other emotional, mental, and physical changes that interfere with daily activities.
One of the key signs of depression is difficulty in getting out of bed and a tendency to oversleep. This is often referred to as "depression napping" or hypersomnia. It is believed that about 15% of people with depression experience hypersomnia. This can be a way to escape emotional pain and is often a physiological effect of the reduction of neurotransmitters common among depressed patients.
While depression is a serious condition, it is manageable. The first step is to recognise the signs and symptoms and seek professional help. A mental health professional can help determine the best treatment plan, which may include therapy, medication, or both.
Treatment Options
Therapy
Several types of counselling can effectively treat depression, including cognitive-behavioural therapy (CBT) and interpersonal therapy (IPT). CBT for insomnia (CBT-I) is a specific type of CBT that focuses on managing chronic insomnia.
Medication
Antidepressant medications can be prescribed to treat depression. It is important to note that these drugs usually take time to improve symptoms, and finding the right medication and dosage may require some trial and error.
Brain Stimulation Therapies
When medications and other approaches are ineffective, brain stimulation therapies such as electroconvulsive therapy (ECT) or emerging methods like repetitive transcranial magnetic stimulation (rTMS) and vagus nerve stimulation (VNS) may be considered.
Self-Care Strategies
In addition to professional treatment, there are also self-care strategies that can help improve sleep quality and manage depression:
- Keeping a consistent sleep schedule by waking up and going to bed at the same time each day.
- Creating a restful nighttime routine and a comfortable sleep environment.
- Avoiding electronic devices before bedtime.
- Skipping heavy meals late in the evening.
- Managing stress levels.
- Limiting caffeine intake, especially later in the day.
- Engaging in regular physical exercise.
Seeking Help
If you or someone you know is struggling with depression, it is important to seek help. Depression is a manageable condition, and with the right treatment and support, it is possible to improve sleep quality and overall well-being.
Sleep Deprivation: The Reason Behind My Gaseous State
You may want to see also
Frequently asked questions
Yes, sleeping all day can be a sign of depression. This condition is called hypersomnia, the opposite of insomnia. It is a common symptom of major depressive disorder, with 65-90% of adult patients experiencing some form of sleep dysfunction.
Hypersomnia is a condition characterised by excessive daytime sleepiness. It is often associated with insomnia, as people with hypersomnia may also find themselves alert and unable to sleep during the day.
Other signs of depression include persistent feelings of sadness, despair, or emptiness; feelings of guilt or worthlessness; loss of interest in activities once enjoyed; changes in eating habits and weight; and thoughts of suicide or death.
If you think you may be experiencing symptoms of depression, it is important to seek professional help. A medical professional can determine whether your symptoms are caused by depression or another health condition. Treatment for depression typically involves a combination of medication and psychotherapy.
Yes, the relationship between sleep and depression is bidirectional. Poor sleep can contribute to the development of depression, and having depression can make a person more likely to experience sleep troubles.