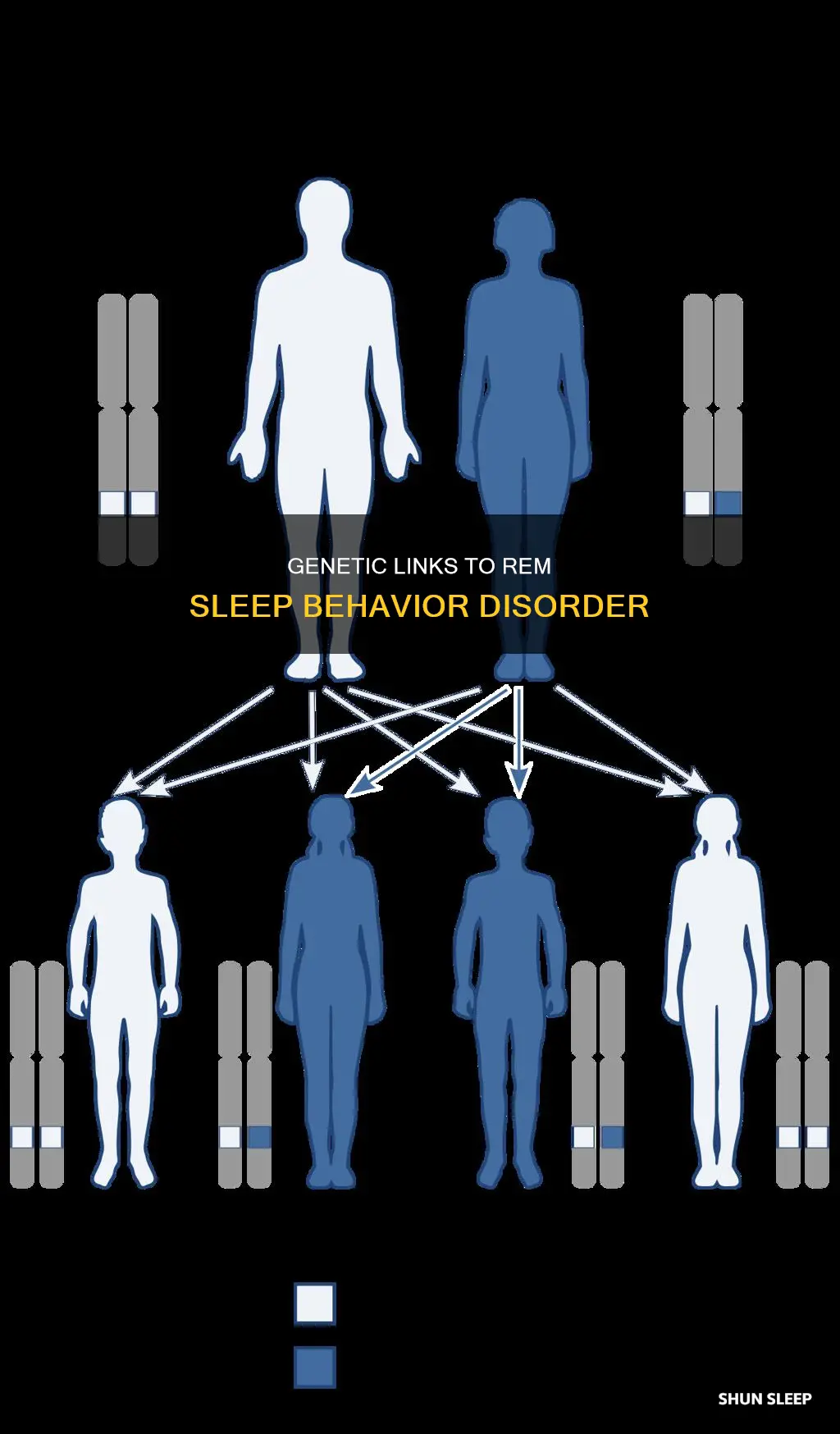
REM sleep behaviour disorder (RBD) is a sleep disorder characterised by abnormal behaviours associated with dream mentation and loss of REM sleep atonia. While the precise genetic causes of RBD are not yet well understood, there is strong evidence of a genetic contribution to the disorder. Over 80% of people with RBD go on to develop a neurodegenerative disorder such as Parkinson's disease or dementia with Lewy bodies. A positive family history of dream enactment was reported in 13.8% of iRBD cases compared to 4.8% of controls. Furthermore, a recent genome-wide association study identified five RBD risk loci near SNCA, GBA, TMEM175, INPP5F, and SCARB2.
| Characteristics | Values |
|---|---|
| Prevalence | Affects about 1% of the general U.S. population and affects 2% of people aged 50 or older |
| Age of onset | The average age of onset is 61 years |
| Gender | Men and people assigned male at birth are nine times more likely than women people assigned female at birth to have RBD |
| Neurodegenerative disorders | About 97% of people who have isolated (idiopathic) RBD will have Parkinson’s disease, Lewy body dementia or multiple system atrophy within 14 years of diagnosis |
| Narcolepsy | Up to 36% of people with Type 1 narcolepsy have secondary (symptomatic) RBD |
| Antidepressants | About 6% of people who take antidepressants have drug-induced RBD |
| Safety measures | Removing sharp, glass and heavy objects away from the bed; placing pillows between the sleeper and surrounding structures; placing a mattress on the floor next to the bed in case the sleeper falls out of bed; sleeping in a sleeping bag |
| Medication | Melatonin, clonazepam and pramipexole can reduce symptoms in some cases |
What You'll Learn
- The genetic link between REM sleep behaviour disorder and synucleinopathies
- The role of the SNCA gene in REM sleep behaviour disorder
- The role of the SCARB2 gene in REM sleep behaviour disorder
- The role of the GBA gene in REM sleep behaviour disorder
- The role of the TMEM175 gene in REM sleep behaviour disorder

The genetic link between REM sleep behaviour disorder and synucleinopathies
REM sleep behaviour disorder (RBD) is characterised by abnormal behaviours during sleep, such as dream enactment, and the loss of muscle atonia during REM sleep. Over 80% of people with RBD go on to develop a synucleinopathy, such as Parkinson's disease or dementia with Lewy bodies. However, the precise role of the SNCA gene, which encodes α-synuclein, has not been well studied.
The SNCA gene and its variants
One study found a variant in the 5′ region of the SNCA gene to be associated with RBD. This variant was also found to be in linkage disequilibrium with other variants in the same region that are associated with various synucleinopathies. However, the role of the SNCA gene in RBD is not yet fully understood, and further research is needed.
The link between RBD and synucleinopathies
Several studies have found a link between RBD and synucleinopathies. One study found that RBD patients were more likely to have a family history of dream enactment, suggesting a possible genetic contribution to RBD. Another study identified five RBD risk loci near the SNCA gene, as well as other genes such as GBA, TMEM175, INPP5F, and SCARB2. These loci have also been implicated in Parkinson's disease, but the RBD-associated variants are independent of those associated with Parkinson's.
The role of RBD in synucleinopathies
RBD is considered a prodromal synucleinopathy, as it often precedes the development of synucleinopathies such as Parkinson's disease, dementia with Lewy bodies, and multiple system atrophy. RBD is also associated with more rapid progression and increased severity of synucleinopathies. Therefore, RBD may be a useful clinical marker for the early detection and treatment of synucleinopathies.
Understanding the Importance of REM Sleep for Restful Nights
You may want to see also

The role of the SNCA gene in REM sleep behaviour disorder
The SNCA gene encodes α-synuclein, the main protein component of Lewy bodies and neurites in synucleinopathies. The precise role of variants in the SNCA gene has not been well studied, but it is known that over 80% of people with REM sleep behaviour disorder (RBD) go on to develop an overt synucleinopathy, such as Parkinson's disease (PD) or dementia with Lewy bodies (DLB).
A 2020 study by Lynne Krohn and colleagues analysed the association between SNCA and RBD in detail. The researchers sequenced SNCA in 1,076 patients with isolated RBD, 1,013 patients with PD, 415 patients with DLB, and 6,155 healthy controls. They found that one variant in the 5′ region of SNCA was associated with RBD and was in linkage disequilibrium with other variants in the same region that are associated with various synucleinopathies.
In a 2022 genome-wide association study, five RBD risk loci were identified near SNCA, GBA, TMEM175, INPP5F, and SCARB2. Expression analyses highlighted SNCA-AS1 and potentially SCARB2 differential expression in different brain regions in RBD, with SNCA-AS1 further supported by colocalization analyses.
A 2021 study found that hypomethylation of intron 1 of the α-synuclein (SNCA) gene has been extensively reported in the blood of patients with α-synucleinopathies. The study assessed blood α-synuclein intron 1 methylation in patients and explored it as a potential biomarker to predict phenoconversion and monitor disease progression. Hypomethylation at cytosine-phosphate-guanine 10, 11, 12, 13, and 17 was found in patients compared with healthy controls. Hypomethylation at cytosine-phosphate-guanine 17 was associated with an increased risk of clinical phenoconversion, which was further enhanced with the presence of subtle motor abnormalities.
Overall, the SNCA gene plays a significant role in RBD and its underlying mechanisms, with several studies identifying links between SNCA variants and an increased risk of RBD and synucleinopathies.
REM Sleep and Sympathetic Nervous System Activity
You may want to see also

The role of the SCARB2 gene in REM sleep behaviour disorder
The SCARB2 gene is one of the five risk loci identified in a genome-wide association study of REM sleep behaviour disorder (RBD). The other four risk loci are SNCA, GBA, TMEM175, and INPP5F. The study found that the RBD-associated SNPs in the SCARB2 gene are not in linkage disequilibrium with the top Parkinson's disease (PD)-associated SNPs in the same loci, and are thus considered independent. The study also found that the RBD risk variant at the SCARB2 locus (rs7697073) is most strongly associated with increased expression in the cortex, while the PD risk variant (rs6825004) is most strongly associated with substantia nigra increased expression.
Accumulating REM Sleep: Adding Up Those Small Moments
You may want to see also

The role of the GBA gene in REM sleep behaviour disorder
The GBA gene is a risk factor for REM sleep behaviour disorder (RBD) and is associated with an increased risk of developing the disorder. The GBA gene is also associated with an earlier age of onset of RBD and an increased rate of conversion to neurodegenerative disease.
The GBA gene encodes the lysosomal enzyme glucocerebrosidase, and variants in this gene are strong and relatively common risk factors for Parkinson's disease and dementia with Lewy bodies. However, their role in multiple system atrophy is unclear.
GBA variants can be classified as severe or mild based on the type of Gaucher disease they are associated with. Severe GBA variants are associated with a higher risk of Parkinson's disease and an earlier average age of onset.
In a study of 1,061 patients with RBD and 3,086 controls, GBA variants were found in 9.5% of patients with RBD compared to 4.1% of controls. The mild p.N370S variant was found in 20 patients with RBD (1.9%) compared to 16 controls (0.5%), while severe variants were found in 6 patients with RBD (0.6%) and 1 control.
Carriers of severe GBA variants had an average age of onset of 52.8 years, 7-8 years earlier than those with mild variants or non-carriers. Of the GBA variant carriers with available data, 52.5% had converted to neurodegenerative disease, compared to 35.6% of non-carriers.
Deep Sleep: Stay Asleep During REM
You may want to see also

The role of the TMEM175 gene in REM sleep behaviour disorder
REM sleep behaviour disorder (RBD) is a prodromal synucleinopathy, with over 80% of patients eventually developing Parkinson's disease, dementia with Lewy bodies, or, in rare cases, multiple system atrophy.
A 2022 genome-wide association study of RBD identified five RBD risk loci near the genes SNCA, GBA, TMEM175, INPP5F, and SCARB2. The study found that RBD-associated SNCA and SCARB2 variants are independent of PD-associated variants in the same loci.
The TMEM175 gene encodes a lysosomal potassium channel. TMEM175 variants have been found to affect the activity of GCase in humans and in vitro. GCase (or glucocerebrosidase) is a lysosomal enzyme that breaks down the lipid glucosylceramide. Mutations in the gene that encodes GCase, GBA, are the most common genetic cause of Parkinson's disease.
TMEM175 variants have been found to affect the age of onset of GBA-associated Parkinson's disease.
The 2022 study found that RBD-associated variants in the TMEM175 locus may affect TMEM175 expression in cortical brain regions.
The study concluded that the lysosomal pathway, and more specifically the GBA pathway, could be a crucial target for therapeutic development to prevent neurodegeneration in RBD.
Twitching in REM Sleep: What Does It Mean?
You may want to see also
Frequently asked questions
REM sleep behaviour disorder (RBD) is a sleep disorder characterised by abnormal behaviours associated with dream mentation and loss of REM sleep atonia.
The symptoms of RBD can vary in severity. While they’re asleep, a person with RBD looks as if they’re acting out a bad dream and may:
- Have mild muscle twitches or limb movements.
- Talk, shout or scream — often using vulgar language.
- Kick, punch or grab the air or their bed partner.
- Jump or fall out of bed.
The main goal of treatment for RBD is to create a safe sleeping environment for you and your bed partner. This can involve certain strategies and medications. Safety measures for RBD include removing sharp, glass and heavy objects away from your bed and placing pillows between you and surrounding structures, such as the headboard or a nightstand.