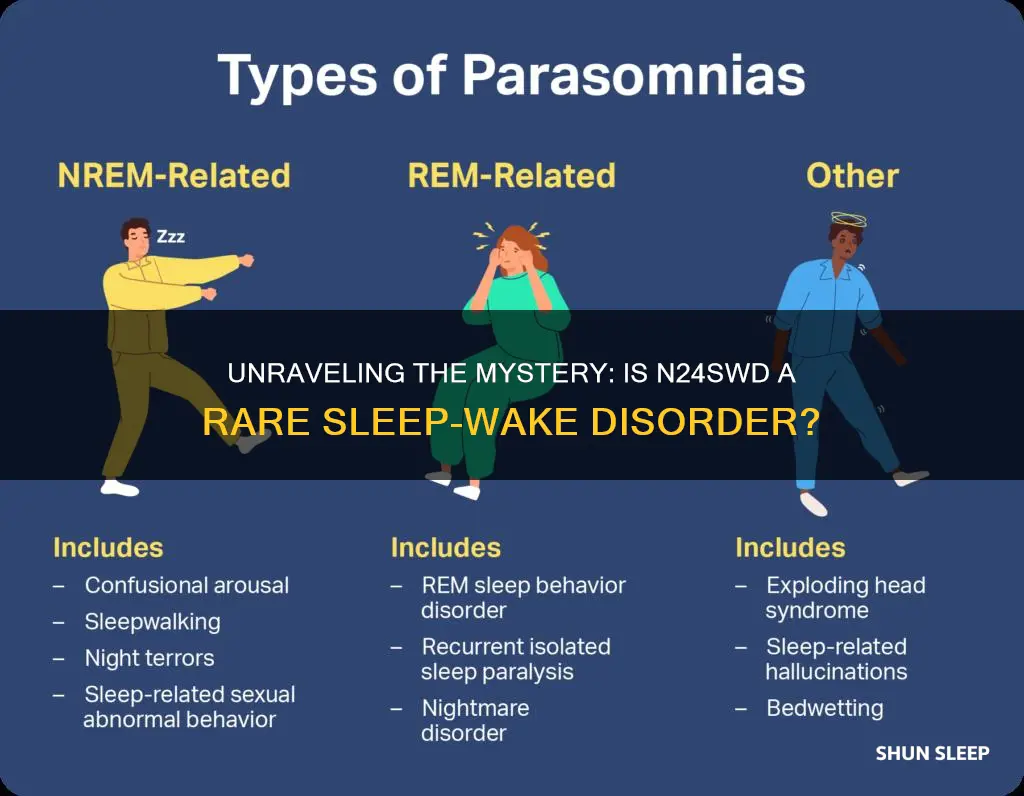
N24SWD, or Non-24-Hour Sleep-Wake Disorder, is a rare and complex sleep disorder that affects the body's internal clock. Unlike typical sleep patterns, individuals with N24SWD experience a misalignment between their sleep-wake cycles and the 24-hour day, leading to significant disruptions in their daily routines. This disorder is often associated with conditions like narcolepsy and can significantly impact an individual's quality of life, making it crucial to understand its characteristics and implications.
| Characteristics | Values |
|---|---|
| Disorder Name | N24SWD (Non-24-Hour Sleep-Wake Disorder) |
| Definition | A circadian rhythm disorder characterized by a misalignment between the body's internal clock and the external 24-hour light-dark cycle. |
| Prevalence | Rare; affects approximately 1 in 100,000 people. |
| Age of Onset | Typically begins in adolescence or early adulthood. |
| Symptoms | - Difficulty falling asleep or staying asleep. - Irregular sleep patterns, often involving excessive daytime sleepiness. - Desynchronization of the body's internal clock with the day-night cycle. - Mood disturbances, including depression and anxiety. |
| Causes | Often associated with a lack of exposure to natural light during the day, especially in individuals with limited access to outdoor activities or those living in indoor environments. |
| Diagnosis | Involves a comprehensive evaluation of sleep patterns, including actigraphy (wearable devices to track movement) and sleep logs. |
| Treatment | - Light therapy: Exposure to bright artificial light during the day to help reset the circadian rhythm. - Melatonin supplements: Used to regulate sleep-wake cycles. - Cognitive-behavioral therapy: Helps individuals manage sleep hygiene and adapt to a new sleep schedule. |
| Prognosis | With proper treatment, many individuals with N24SWD can improve their sleep patterns and overall quality of life. |
| Research Focus | Understanding the underlying mechanisms and developing more effective treatment strategies. |
What You'll Learn
- Definition: N24SWD is a rare sleep-wake disorder characterized by irregular sleep patterns
- Symptoms: Patients experience excessive daytime sleepiness and disrupted night sleep
- Diagnosis: It's diagnosed through sleep studies and patient interviews
- Treatment: Treatment focuses on improving sleep hygiene and managing symptoms
- Research: Little is known about the prevalence and causes of N24SWD

Definition: N24SWD is a rare sleep-wake disorder characterized by irregular sleep patterns
N24SWD, or Non-24-Hour Sleep-Wake Disorder, is a rare and complex condition that disrupts the natural sleep-wake cycle of individuals. This disorder is often referred to as a circadian rhythm disorder, as it affects the body's internal clock, which regulates the timing of sleep and wakefulness. People with N24SWD experience a misalignment between their sleep patterns and the standard 24-hour day, leading to significant challenges in their daily lives.
The core feature of this disorder is the irregularity of sleep cycles. Individuals with N24SWD may go to bed and wake up at various times, often feeling more alert during the night and struggling to fall asleep during the day. Their sleep patterns can vary widely, making it difficult to establish a consistent routine. For example, someone with this disorder might fall asleep at 2 am and wake up at 10 am, only to feel the need to nap again in the early afternoon. This irregularity can lead to excessive daytime sleepiness, impaired cognitive function, and a reduced quality of life.
This disorder is considered rare because it affects a small percentage of the population. It is more commonly observed in individuals who have experienced disruptions to their natural circadian rhythms, such as those working night shifts or those with a history of jet lag. The exact cause of N24SWD is not fully understood, but it is believed to be related to the body's natural circadian rhythm and its sensitivity to external factors.
Diagnosing N24SWD can be challenging due to its unique presentation. Healthcare professionals often use a combination of methods, including sleep diaries, actigraphy (a non-invasive device to track sleep-wake cycles), and specialized sleep studies, to identify the irregular sleep patterns characteristic of this disorder. Treatment options aim to synchronize the individual's sleep-wake cycle with the standard day-night rhythm, often involving gradual adjustments to sleep schedules and, in some cases, the use of bright light therapy.
In summary, N24SWD is a rare sleep-wake disorder that disrupts the natural sleep patterns of affected individuals. Its irregularity and complexity make it a challenging condition to manage, requiring specialized diagnostic and treatment approaches to help individuals regain a healthy sleep-wake cycle.
Maximizing Naps: Does Wake-to-Sleep Enhance Your Rest?
You may want to see also

Symptoms: Patients experience excessive daytime sleepiness and disrupted night sleep
The condition you're referring to, N24SWD (Non-24-Hour Sleep-Wake Disorder), is a unique and complex sleep disorder that primarily affects individuals who are completely blind. It is a circadian rhythm disorder, meaning it is a problem with the body's internal clock that regulates sleep and wake cycles. Patients with N24SWD experience a misalignment between their internal body clock and the external 24-hour light-dark cycle, leading to significant disruptions in their sleep-wake patterns.
One of the most prominent symptoms of N24SWD is excessive daytime sleepiness. Patients often feel an overwhelming need to sleep during the day, even when they have had a full night's rest. This can make it extremely challenging for them to stay awake during the day, affecting their ability to perform daily activities, work, and maintain social interactions. The excessive sleepiness is not due to poor sleep quality at night but rather the body's inability to synchronize with the standard day-night cycle.
Night sleep is also significantly impacted in individuals with N24SWD. Their sleep patterns are often fragmented, and they may experience insomnia or frequent awakenings during the night. Despite feeling very tired, they might struggle to fall asleep at the typical bedtime and may need to adjust their sleep schedules to align with their internal body clock. This disruption in night sleep can lead to a vicious cycle, where the lack of restorative sleep during the night further exacerbates the daytime sleepiness.
The symptoms of N24SWD can vary among patients, and some individuals may experience more severe disruptions than others. The disorder can significantly impact a person's quality of life, affecting their overall health, mood, and ability to function in daily activities. It is important for patients to work closely with healthcare professionals to manage these symptoms and find appropriate treatment options.
Managing N24SWD often involves a multidisciplinary approach, including sleep specialists, ophthalmologists, and other healthcare providers. Treatment strategies may include light therapy, where patients are exposed to specific types of light at controlled times to help reset their internal body clock. Other interventions might include medication adjustments, sleep hygiene education, and behavioral therapies to improve sleep quality and reduce excessive daytime sleepiness.
Does Yelling Wake Up a Sleeping PC in D&D 5e?
You may want to see also

Diagnosis: It's diagnosed through sleep studies and patient interviews
The diagnosis of N24SWD (Non-24-Hour Sleep-Wake Disorder), a rare circadian rhythm sleep-wake disorder, involves a comprehensive approach that includes both sleep studies and patient interviews. This multi-faceted process is crucial in understanding the unique sleep patterns and challenges faced by individuals with this condition.
Sleep studies, often conducted in specialized sleep laboratories, are a fundamental part of the diagnostic process. During these studies, patients spend one or more nights in a controlled environment where their sleep patterns are closely monitored. This involves the use of various tools such as polysomnography, which records brain waves, eye movements, muscle activity, heart rate, and breathing. The data collected from these studies provides valuable insights into the patient's sleep architecture, including sleep stages, sleep-wake transitions, and any disruptions in their natural sleep-wake cycle.
In addition to sleep studies, patient interviews play a pivotal role in the diagnosis. Healthcare professionals conduct detailed interviews to gather information about the patient's sleep history, daily routines, and any symptoms they experience. These interviews help identify patterns and triggers that may contribute to the disorder. Patients are encouraged to share their experiences, including any difficulties they face in maintaining a consistent sleep schedule, their energy levels throughout the day, and any behavioral or environmental factors that might influence their sleep.
The combination of sleep studies and patient interviews allows for a comprehensive understanding of the individual's sleep-wake patterns and the impact of N24SWD on their daily life. This information is crucial for healthcare providers to make an accurate diagnosis and develop a tailored treatment plan. It also helps in ruling out other potential sleep disorders or medical conditions that might present similar symptoms.
Furthermore, the diagnostic process may involve ruling out other circadian rhythm disorders and ensuring that the patient's symptoms are not better explained by other sleep-related conditions. This meticulous approach ensures that individuals with N24SWD receive the appropriate care and support to manage their unique sleep challenges effectively.
Mastering Remote Wake-Up: Unlock Windows 10's Sleep Override
You may want to see also

Treatment: Treatment focuses on improving sleep hygiene and managing symptoms
The treatment approach for individuals with N24SWD (Non-24-Hour Sleep-Wake Disorder) primarily aims to enhance sleep hygiene and effectively manage its associated symptoms. This condition is a unique circadian rhythm disorder that disrupts the natural sleep-wake cycle, often affecting individuals with advanced sleep phase syndrome. Here's an overview of the treatment strategies:
Sleep Hygiene Improvement: Establishing a consistent sleep schedule is crucial. Patients are advised to go to bed and wake up at the same time every day, even on weekends. This routine helps regulate the body's internal clock. Maintaining a relaxing bedtime routine, ensuring a comfortable sleep environment, and avoiding stimulants like caffeine close to bedtime are essential components of sleep hygiene. Encouraging regular physical activity during the day can also promote better sleep at night.
Light Therapy: Light exposure plays a significant role in treating N24SWD. During the day, especially in the morning, exposure to bright light helps synchronize the body's circadian rhythm. This can be achieved through natural sunlight or specialized light therapy boxes. Gradually adjusting the timing of light exposure can help shift the sleep-wake cycle. It is recommended to use light therapy under professional guidance to ensure the correct duration and intensity of light exposure.
Sleep Restriction Therapy: This technique involves gradually reducing the amount of time spent in bed to match the patient's actual sleep needs. By limiting the time in bed, the body's sleep drive increases, leading to improved sleep efficiency. This method is particularly useful for individuals who struggle with insomnia and can help regulate the sleep-wake cycle.
Symptom Management: Managing symptoms is an essential part of treatment. Medications may be prescribed to help regulate sleep, especially when light therapy alone is insufficient. Melatonin, a hormone that regulates sleep, is often used to adjust the sleep-wake cycle. Additionally, cognitive-behavioral therapy (CBT) can be beneficial in addressing any underlying psychological issues related to sleep disturbances.
Lifestyle Adjustments: Making lifestyle changes can significantly impact managing N24SWD. This includes maintaining a regular exercise routine, as physical activity can improve sleep quality. Avoiding napping during the day, especially in the afternoon and evening, is crucial to prevent further disruption of the sleep-wake cycle. Creating a calm and quiet environment for sleep can also improve overall sleep hygiene.
In summary, treating N24SWD involves a comprehensive approach, combining sleep hygiene practices, light therapy, and symptom management techniques. It is essential to tailor the treatment plan to individual needs, as each person's experience with this disorder may vary. With proper management, many individuals with N24SWD can improve their sleep patterns and overall quality of life.
Restless Nights: Unraveling the Mystery of Insomnia and Heart Palpitations
You may want to see also

Research: Little is known about the prevalence and causes of N24SWD
The term "N24SWD" is not a widely recognized medical acronym, and as such, it is challenging to provide specific details about its prevalence and causes. However, based on the context of your request, it appears that N24SWD might be a newly proposed or less common sleep disorder. Here is a structured overview of the research landscape regarding this condition:
Prevalence and Incidence: Research on N24SWD is limited, and there is a dearth of studies specifically addressing its prevalence in the general population. Most sleep wake disorders are relatively well-studied, but this particular condition seems to have received little attention from researchers. The lack of comprehensive data makes it difficult to determine whether N24SWD is indeed rare or if it simply hasn't been extensively investigated.
Causes and Risk Factors: Understanding the causes and risk factors associated with N24SWD is even more challenging due to the scarcity of research. Sleep disorders often have complex etiology, involving genetic, environmental, and psychological factors. Without specific studies, it is impossible to identify potential triggers or predisposing conditions for N24SWD. This knowledge gap hinders the development of effective prevention strategies and targeted treatments.
Diagnosis and Classification: The absence of a widely accepted diagnostic criteria for N24SWD further complicates research efforts. Sleep medicine relies on standardized diagnostic tools and classification systems to ensure consistency in research and clinical practice. Without a clear definition and diagnostic framework, researchers face challenges in identifying and studying cases of N24SWD, making it difficult to contribute to the broader understanding of sleep disorders.
Future Directions for Research: Given the limited information available, it is essential to prioritize research into N24SWD. This includes conducting epidemiological studies to estimate its prevalence, identifying potential risk factors, and developing standardized diagnostic criteria. By addressing these knowledge gaps, researchers can contribute to a more comprehensive understanding of sleep disorders, improve diagnostic accuracy, and ultimately enhance patient care and management.
In summary, the term N24SWD, as it stands, lacks sufficient research to provide concrete answers about its prevalence and causes. However, the absence of detailed information highlights the need for further investigation to better understand this potential sleep wake disorder and its impact on affected individuals.
Revive Your Student's Energy: Strategies to Wake Up and Focus
You may want to see also
Frequently asked questions
Narcolepsy is a chronic neurological disorder that affects the brain's ability to regulate sleep-wake cycles. It is characterized by excessive daytime sleepiness, sudden muscle weakness (cataplexy), sleep paralysis, and hallucinations.
Narcolepsy is considered a rare disorder, with an estimated prevalence of about 1 in 2,000 people in the United States. However, it is often underdiagnosed, and many individuals may not be aware they have the condition.
The exact cause of Narcolepsy is not fully understood, but it is believed to be related to a combination of genetic and environmental factors. It is often associated with a deficiency in a neurotransmitter called hypocretin, which helps regulate sleep and wakefulness.
While there is no cure for Narcolepsy, various treatments can help manage symptoms. These may include stimulant medications to promote wakefulness, sleep hygiene practices, cognitive-behavioral therapy, and in some cases, surgical interventions.
Yes, Narcolepsy can be classified into two main types: Narcolepsy type 1 (NT1) and Narcolepsy type 2 (NT2). NT1 is often associated with a complete loss of hypocretin-producing neurons, while NT2 may have a partial deficiency. Both types can lead to similar symptoms but may have different underlying causes and progression.