Sleep paralysis and a wake-up stroke are two distinct but related phenomena that can occur during the transition between sleep and wakefulness. While a wake-up stroke refers to a sudden, involuntary movement of the body that can occur when falling asleep, sleep paralysis involves a temporary inability to move or speak that can happen when falling asleep or waking up. Both conditions can be unsettling and may involve hallucinations or a sense of dread. Understanding the differences between these experiences is important for recognizing and addressing any potential underlying issues related to sleep quality and mental health.
What You'll Learn
- Definition of Sleep Paralysis: A temporary inability to move or speak during sleep, often accompanied by vivid hallucinations
- Wake-Up Stroke vs. Sleep Paralysis: A wake-up stroke is a medical emergency, while sleep paralysis is a sleep disorder
- Symptoms of Sleep Paralysis: Hallucinations, fear, inability to move or speak, and a sense of suffocation
- Duration of Sleep Paralysis: Episodes can last from a few seconds to several minutes, rarely longer
- Treatment and Prevention: Seeking medical help for wake-up strokes; managing sleep hygiene for sleep paralysis

Definition of Sleep Paralysis: A temporary inability to move or speak during sleep, often accompanied by vivid hallucinations
Sleep paralysis is a fascinating yet often distressing phenomenon that can occur during the transition between sleep and wakefulness. It is a state where an individual becomes conscious but is temporarily unable to move or speak, often accompanied by a sense of fear and intense hallucinations. This experience can be particularly terrifying as it may feel like one is being trapped or unable to escape a terrifying presence.
During an episode of sleep paralysis, a person's mind is alert and aware, but their body remains paralyzed, similar to the state of paralysis experienced during REM sleep. This paralysis is a natural mechanism to prevent acting out dreams and potential harm to oneself or others. However, in sleep paralysis, this paralysis persists even after the individual is awake, causing a sense of being trapped in a state of immobility. The hallucinations that accompany this condition can be highly realistic and often involve a presence in the room, feeling a weight on one's chest, or experiencing a sense of suffocation. These hallucinations can vary widely and may include visual, auditory, or even tactile sensations, making the experience incredibly vivid and intense.
The duration of sleep paralysis episodes can range from a few seconds to several minutes, and they often occur upon falling asleep or waking up. It is a relatively common occurrence, affecting a significant portion of the population at some point in their lives. While it can be a frightening experience, it is generally not harmful and typically resolves on its own. However, for some individuals, it may lead to persistent anxiety or sleep disturbances, especially if they have frequent or severe episodes.
Understanding sleep paralysis is essential as it can help individuals recognize and manage the condition. It is different from a stroke, which is a medical emergency characterized by sudden symptoms such as paralysis, speech difficulties, or severe headache. Sleep paralysis, while distressing, is a sleep disorder and not a medical emergency. Recognizing the difference between these conditions is crucial for proper diagnosis and treatment.
In summary, sleep paralysis is a temporary state of consciousness with an inability to move or speak, often accompanied by vivid hallucinations. It is a unique and sometimes frightening experience that can occur during the transition between sleep and wakefulness. By understanding its definition and characteristics, individuals can better manage and cope with this phenomenon.
Troubleshooting: Dell Desktop Won't Wake from Sleep Mode
You may want to see also

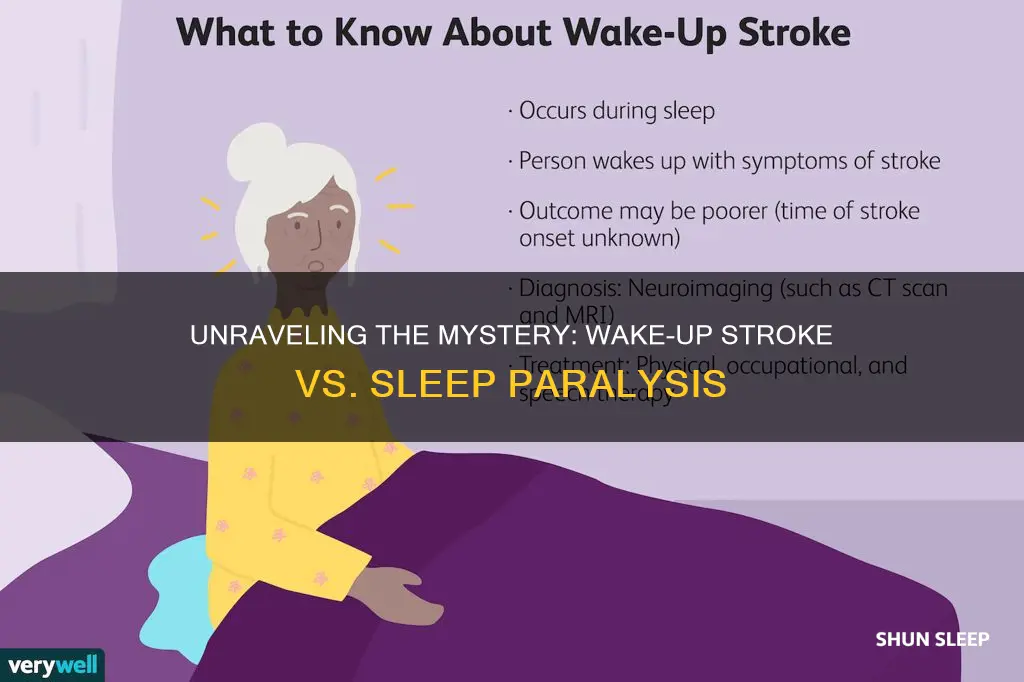
Wake-Up Stroke vs. Sleep Paralysis: A wake-up stroke is a medical emergency, while sleep paralysis is a sleep disorder
A wake-up stroke and sleep paralysis are two distinct medical conditions that often get confused due to their similar names and some overlapping symptoms. However, understanding the differences between these two phenomena is crucial for proper diagnosis and treatment.
Wake-Up Stroke:
A wake-up stroke, also known as a sleep-related stroke, occurs when a person has a stroke while sleeping. This type of stroke is a medical emergency and requires immediate attention. During a wake-up stroke, the blood flow to the brain is interrupted, leading to brain cell damage and potential long-term consequences. Symptoms can include sudden weakness or numbness in the face, arm, or leg, especially on one side of the body; difficulty speaking or understanding speech; sudden vision changes; and a severe headache without an apparent cause. It is essential to recognize these signs and seek emergency medical care as quickly as possible, as prompt treatment can significantly improve outcomes.
Sleep Paralysis:
Sleep paralysis, on the other hand, is a sleep disorder that affects the mind's ability to act while the body is paralyzed during the transition between sleep and wakefulness. This condition is often associated with narcolepsy and occurs when a person becomes conscious but is temporarily unable to move or speak. During an episode of sleep paralysis, individuals may experience a sense of being unable to breathe, a feeling of being suffocated, or an overwhelming fear. It is important to note that sleep paralysis is not a medical emergency and typically resolves on its own within a few minutes. However, it can be a distressing experience and may require management strategies to cope with the symptoms.
While both conditions can be alarming, they require different approaches. Wake-up strokes demand immediate medical attention to prevent irreversible brain damage, whereas sleep paralysis is a sleep-related phenomenon that can be managed with proper sleep hygiene and, in some cases, medication. Recognizing the unique characteristics of each condition is essential for individuals to seek the appropriate care and ensure the best possible health outcomes.
Revive Your MacBook: Tips to Wake Up a Slumbering Machine
You may want to see also

Symptoms of Sleep Paralysis: Hallucinations, fear, inability to move or speak, and a sense of suffocation
Sleep paralysis is a fascinating yet often terrifying phenomenon that can occur during the transition between sleep and wakefulness. It is a state where an individual becomes conscious but is temporarily unable to move or speak, often accompanied by a range of distressing symptoms. This condition can be a result of various factors, including sleep deprivation, irregular sleep patterns, and certain medical conditions. Understanding the symptoms is crucial for recognizing and managing this experience effectively.
One of the most common symptoms of sleep paralysis is the inability to move or speak. When an individual experiences this, they may feel completely paralyzed, as if their body is heavy and immobile. This sensation can be incredibly frightening, especially when it occurs in the middle of the night, leaving one aware but unable to act. The paralysis typically affects the entire body, making it impossible to sit up, walk, or even blink. Interestingly, the mind remains alert, and the person is fully conscious, often aware of their surroundings, which intensifies the sense of dread.
Hallucinations are another distressing aspect of sleep paralysis. These can be visual, auditory, or even tactile hallucinations. Visual hallucinations may include seeing shadows, figures, or monsters in the room. Auditory hallucinations might involve hearing voices, whispers, or strange noises. Tactile hallucinations could manifest as a feeling of something touching or pressing against the body, often described as a suffocating or oppressive sensation. These hallucinations can be incredibly realistic and may trigger intense fear and confusion.
Fear is a prevalent emotion during sleep paralysis episodes. The inability to move or speak, coupled with vivid hallucinations, can induce a sense of panic and terror. Individuals may feel a profound sense of dread, as if they are trapped and unable to escape. The fear can be so overwhelming that it becomes challenging to distinguish between the real and the imagined, further exacerbating the distress. It is not uncommon for people to believe they are experiencing a genuine medical emergency or even a supernatural occurrence.
A sense of suffocation is also frequently reported during sleep paralysis. This feeling can be attributed to the physical paralysis and the associated hallucinations. The individual may perceive their throat or chest as being compressed, making it difficult to breathe. This sensation, combined with the fear and inability to move, can create a powerful and distressing experience. Many people describe it as a terrifying nightmare, leaving them feeling anxious and vulnerable upon awakening.
Recognizing these symptoms is essential for individuals who have experienced sleep paralysis to understand that they are not alone and that there are ways to manage and cope with these episodes. While it can be a frightening experience, seeking support and learning about sleep hygiene practices can help reduce the frequency and intensity of sleep paralysis episodes.
Revive Your Screen: Tips to Wake Up Your Device from Sleep Mode
You may want to see also

Duration of Sleep Paralysis: Episodes can last from a few seconds to several minutes, rarely longer
Sleep paralysis is a fascinating yet often unsettling phenomenon that can occur during the transition between sleep and wakefulness. It is characterized by a temporary inability to move or speak, often accompanied by intense feelings of fear and a sense of presence in the room. This experience can last from a few seconds to several minutes, and it is a rare occurrence for it to extend beyond this duration.
During an episode of sleep paralysis, individuals may find themselves fully awake but unable to move their bodies, a condition known as cataplexy. This paralysis can affect the entire body or specific muscle groups, and it is often described as a feeling of being paralyzed by an external force. The duration of this paralysis varies, but it typically resolves within a short time frame. Some individuals may experience a rapid return to normalcy, while others might have a gradual release from the paralysis.
The duration of sleep paralysis episodes is influenced by various factors. Firstly, the quality of sleep leading up to the episode plays a significant role. Individuals who have disrupted sleep patterns or are sleep-deprived may be more susceptible to longer episodes. Additionally, the intensity of the fear and the individual's psychological state can impact the length of the experience. In some cases, the mind's struggle to understand the situation can prolong the paralysis.
It is important to note that sleep paralysis is a relatively rare occurrence and is not typically associated with any serious health risks. However, the intense emotions and physical sensations experienced during an episode can be distressing. Many people who experience sleep paralysis report feeling a sense of dread and a need to escape the situation. The duration of these episodes can vary widely, and understanding this variability can help individuals manage their expectations and reactions.
In summary, sleep paralysis episodes can range from brief moments of paralysis to longer durations, but they rarely exceed several minutes. The experience can be unsettling, and individuals may feel a sense of urgency to regain control. Recognizing the factors that influence the duration of these episodes can provide valuable insights for those who have experienced or are studying sleep paralysis.
Revive Your Computer: Tips to Wake Up a Slumbering Machine
You may want to see also

Treatment and Prevention: Seeking medical help for wake-up strokes; managing sleep hygiene for sleep paralysis
Understanding the distinction between wake-up strokes and sleep paralysis is crucial for proper treatment and management. While both conditions can be alarming and may share some symptoms, they are distinct medical conditions that require different approaches.
Seeking Medical Help for Wake-Up Strokes:
When an individual experiences a wake-up stroke, it is essential to act quickly. Wake-up strokes are a type of stroke that occurs when a blood vessel in the brain bursts or becomes blocked, leading to a sudden loss of function in the brain. These strokes often present with symptoms such as sudden weakness or numbness on one side of the body, difficulty speaking or understanding speech, severe headache, and loss of balance. If you or someone you know is experiencing these symptoms, it is imperative to call emergency services immediately. Time is critical in stroke treatment, and the faster medical intervention occurs, the better the chances of minimizing brain damage and improving recovery. Upon arrival at the hospital, medical professionals will conduct a series of tests, including brain imaging, to confirm the diagnosis and determine the appropriate treatment plan. Treatment options may include medications to dissolve blood clots, surgical procedures to remove blood clots or blocked vessels, and rehabilitation therapies to help restore function and improve recovery.
Managing Sleep Hygiene for Sleep Paralysis:
Sleep paralysis, on the other hand, is a sleep disorder characterized by a state of consciousness during which the individual is unable to move their body while experiencing hallucinations and a sense of fear or dread. It often occurs during the transition between sleep and wakefulness, making it challenging to distinguish from a waking state. To manage sleep paralysis, improving sleep hygiene is essential. Here are some strategies:
- Establish a Consistent Sleep Schedule: Go to bed and wake up at the same time every day, even on weekends. This helps regulate your body's internal clock and promotes better sleep quality.
- Create a Relaxing Bedtime Routine: Engage in calming activities before bed, such as reading, light stretching, or listening to soothing music. Avoid stimulating activities like intense exercise or watching thrilling movies close to bedtime.
- Optimize Your Sleep Environment: Ensure your bedroom is cool, dark, and quiet. Invest in comfortable bedding and consider using earplugs or white noise machines to create a peaceful sleep environment.
- Limit Stimulants and Screens: Reduce caffeine and nicotine intake, especially in the afternoon and evening. Minimize exposure to electronic devices, especially before bed, as the blue light emitted can interfere with your sleep-wake cycle.
- Practice Relaxation Techniques: Incorporate relaxation practices such as deep breathing exercises, meditation, or progressive muscle relaxation into your daily routine. These techniques can help reduce stress and improve overall sleep quality.
In both cases, seeking professional medical advice is paramount. For wake-up strokes, prompt medical attention can significantly improve outcomes, and for sleep paralysis, understanding the underlying causes and managing sleep hygiene can help reduce the frequency and intensity of episodes. Remember, early intervention and proper management are key to effectively addressing these conditions.
Overcoming the Night Sweats: Tips for a Restful Sleep
You may want to see also
Frequently asked questions
A wake-up stroke, also known as sleep paralysis, is a sleep disorder that occurs when a person becomes conscious but is unable to move or speak for a brief period. It happens when the body's muscles remain paralyzed at the transition between sleep and wakefulness, often causing a sense of fear or distress. While both conditions involve a loss of motor control, a wake-up stroke is a medical emergency and requires immediate attention, whereas sleep paralysis is a temporary and relatively common sleep phenomenon.
Sleep paralysis is a fascinating yet unsettling experience. It typically occurs during the REM (rapid eye movement) stage of sleep when the body's muscles are temporarily paralyzed to prevent acting out dreams. When a person experiences sleep paralysis, they are fully awake but cannot move or speak, often feeling a sense of pressure or weight on their chest. This can be accompanied by vivid hallucinations, where they may see threatening figures or hear voices. It usually lasts for a few minutes before the person regains control over their body.
Both conditions are related to the transition between sleep and wakefulness and can cause a loss of motor control. However, a wake-up stroke is a medical emergency and may indicate a serious underlying health issue, such as a heart attack or a stroke. It often involves a sudden loss of consciousness and can be life-threatening. Sleep paralysis, on the other hand, is a sleep disorder that can occur in individuals without any known medical conditions and is generally not life-threatening, although it can be extremely distressing.