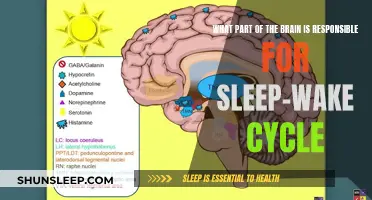
Vertigo, a sensation of spinning or feeling off-balance, can significantly impact one's daily life, and its effects may extend to sleep as well. Many individuals with vertigo experience disruptions in their sleep patterns, often waking up frequently or struggling to fall asleep. This phenomenon can be attributed to the underlying causes of vertigo, such as inner ear issues, brain injuries, or neurological disorders. Understanding the relationship between vertigo and sleep is crucial for managing symptoms and improving overall well-being.
What You'll Learn
- Vertigo's Impact on Sleep Patterns: How vertigo disrupts sleep cycles and affects overall rest quality
- Triggering Factors: Common triggers like sudden head movements or specific sleep positions
- Sleep Disorders: Vertigo's association with conditions like insomnia and sleep apnea
- Management Strategies: Techniques to manage vertigo symptoms during sleep, such as positional therapy
- Medical Interventions: Exploring treatments and therapies to alleviate vertigo and improve sleep

Vertigo's Impact on Sleep Patterns: How vertigo disrupts sleep cycles and affects overall rest quality
Vertigo, a sensation of spinning or feeling off-balance, can significantly impact one's sleep patterns and overall rest quality. It is a symptom that often arises from issues within the inner ear or brain, and its effects on sleep can be quite disruptive. Many individuals with vertigo experience a constant sense of imbalance, which can lead to frequent awakenings during the night, making it challenging to achieve a deep and restful sleep.
During sleep, our bodies naturally go through different stages, including non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. These stages are crucial for restorative functions and cognitive processing. However, vertigo can interfere with this natural sleep cycle. When an individual experiences vertigo, the spinning sensation can trigger sudden movements or a desire to correct the perceived imbalance, causing them to wake up. This disruption in the sleep cycle can lead to a fragmented sleep pattern, where the quality of rest is compromised.
The impact of vertigo on sleep is twofold. Firstly, the initial awakening can disrupt the first stage of NREM sleep, which is essential for falling into a deep sleep. This stage is characterized by slow brain waves and muscle relaxation, and any interruption can lead to increased sleep fragmentation. Secondly, the recurrent awakenings caused by vertigo can prevent individuals from reaching the deeper stages of sleep, including REM sleep, which is vital for memory consolidation and emotional processing. As a result, people with vertigo may experience frequent arousals, leaving them feeling unrefreshed and fatigued during the day.
The consequences of disrupted sleep due to vertigo can be far-reaching. Lack of quality sleep can contribute to cognitive impairments, such as difficulty concentrating, impaired judgment, and reduced problem-solving abilities. It can also affect mood and emotional regulation, leading to increased irritability, anxiety, or depression. Furthermore, over time, chronic sleep deprivation can weaken the immune system, making individuals more susceptible to illnesses and affecting their overall health and well-being.
Managing vertigo and its impact on sleep is essential for improving overall health. Treatment options may include vestibular rehabilitation therapy, which aims to retrain the brain's response to vertigo, and various medications to alleviate symptoms. Additionally, creating a sleep-friendly environment, such as ensuring a comfortable mattress and pillows, minimizing noise and light disturbances, and establishing a consistent sleep schedule, can significantly contribute to better sleep quality for individuals dealing with vertigo.
Fitbit Versa's Wake-Up Feature: Does It Work in Light Sleep?
You may want to see also

Triggering Factors: Common triggers like sudden head movements or specific sleep positions
Vertigo, a sensation of spinning or feeling off-balance, can indeed disrupt sleep and cause sudden awakenings. One of the primary triggers for vertigo during sleep is sudden head movements. When you move your head rapidly, especially during the night, it can stimulate the inner ear's balance mechanisms, leading to a vertigo episode. This is particularly common in individuals with conditions like benign paroxysmal positional vertigo (BPPV), where small crystals in the inner ear become dislodged, causing sudden and intense vertigo spells. A sudden head turn or roll can trigger these crystals to move, resulting in a sudden onset of vertigo that may wake you from a deep sleep.
Additionally, certain sleep positions can exacerbate vertigo symptoms. For instance, sleeping on your back may cause the cerebrospinal fluid in the inner ear to shift, potentially triggering vertigo. Similarly, lying on your side with your head positioned at the edge of the bed can also lead to sudden head movements, especially if you roll over abruptly. These movements can stimulate the vestibular system, which is responsible for balance, and may result in a vertigo attack that disrupts your sleep.
To minimize the impact of these triggers, consider adjusting your sleep position and movements. Sleeping on your side with a pillow between your knees can help maintain a stable position and reduce sudden head movements. Alternatively, using a body pillow or a regular pillow to support your neck and head can provide better alignment and reduce the risk of vertigo episodes during sleep.
It is also beneficial to establish a consistent sleep routine and create a sleep-friendly environment. Avoid consuming caffeine or alcohol close to bedtime, as these substances can disrupt sleep quality and potentially exacerbate vertigo symptoms. Instead, opt for a warm bath or some light reading before bed to signal to your body that it's time to wind down.
In some cases, managing vertigo during sleep may require medical intervention. If sudden head movements or specific sleep positions consistently trigger vertigo, consulting an ENT (Ear, Nose, and Throat) specialist or a neurologist can provide valuable insights and treatment options. They may recommend specific exercises, such as the Epley maneuver for BPPV, or suggest other therapies to help manage and reduce the frequency of vertigo episodes.
Deep Sleep, Wake-Up Calls: The Watchdog Effect
You may want to see also

Sleep Disorders: Vertigo's association with conditions like insomnia and sleep apnea
Vertigo, a sensation of spinning or feeling off-balance, can significantly impact one's quality of life, especially when it disrupts sleep. While it is often associated with physical conditions like inner ear problems or neurological disorders, its relationship with sleep disorders is an intriguing aspect that warrants exploration. This article delves into how vertigo can be linked to insomnia and sleep apnea, offering insights into the complex interplay between these conditions.
Vertigo and Insomnia: A Complex Relationship
Insomnia, characterized by difficulty falling asleep or staying asleep, can often be accompanied by episodes of vertigo. This association is particularly intriguing as it suggests a potential bidirectional relationship between the two conditions. Individuals with insomnia may experience vertigo as a result of prolonged periods of sleep deprivation, which can lead to increased stress and anxiety. These emotional and physiological changes may then trigger vertigo symptoms, creating a vicious cycle. For instance, the anxiety and restlessness associated with insomnia can cause muscle tension, which, in turn, may lead to vertigo episodes.
Moreover, the impact of insomnia on the body's natural circadian rhythm can also contribute to vertigo. The body's internal clock, which regulates sleep-wake cycles, can become disrupted in individuals with insomnia. This disruption may result in an imbalance in the body's natural release of neurotransmitters and hormones, potentially triggering vertigo. The complex interplay between sleep deprivation, emotional stress, and physiological changes makes the relationship between insomnia and vertigo a challenging one to unravel.
Vertigo and Sleep Apnea: A Noisy Connection
Sleep apnea, a sleep disorder characterized by pauses in breathing during sleep, shares a unique connection with vertigo. Individuals with sleep apnea often experience fragmented sleep, which can lead to frequent awakenings throughout the night. These awakenings can be sudden and intense, often accompanied by a feeling of disorientation and imbalance, which are classic symptoms of vertigo. The lack of restorative sleep in sleep apnea patients can contribute to the development of vertigo, making it a significant comorbidity.
The relationship between sleep apnea and vertigo is further complicated by the physical and physiological changes that occur during sleep apnea episodes. The repeated pauses in breathing can lead to oxygen deprivation, causing headaches, dizziness, and a sense of unsteadiness. These symptoms can persist even after the individual has awakened, contributing to the vertigo-like sensations experienced during the day. Additionally, the treatment of sleep apnea, such as the use of continuous positive airway pressure (CPAP) machines, can sometimes cause side effects like nasal congestion and dry mouth, which may indirectly contribute to vertigo symptoms.
Understanding the Underlying Mechanisms
The association between vertigo and sleep disorders like insomnia and sleep apnea highlights the intricate relationship between sleep and balance. Both conditions share common underlying mechanisms that contribute to their symptoms. For instance, the body's autonomic nervous system, which regulates involuntary bodily functions, plays a crucial role in both vertigo and sleep disorders. Dysregulation of this system can lead to the symptoms experienced in both conditions.
Furthermore, the impact of sleep disorders on the brain's cognitive functions cannot be overlooked. Sleep deprivation and disrupted sleep patterns can affect the brain's ability to process information and maintain balance. This cognitive impairment can lead to the development of vertigo symptoms, making it a significant factor in the relationship between sleep disorders and vertigo. Understanding these underlying mechanisms is essential for developing effective treatment strategies that address both the sleep disorder and the associated vertigo.
The association between vertigo and sleep disorders like insomnia and sleep apnea underscores the importance of a comprehensive approach to treatment. Addressing one condition without considering the other may not provide optimal relief for the patient. For instance, treating insomnia without addressing the underlying sleep apnea can lead to persistent vertigo symptoms. Similarly, managing vertigo without addressing the sleep disorder may not address the root cause of the issue.
A holistic approach, which considers the interplay between sleep, balance, and cognitive functions, is essential. This may involve a multidisciplinary team of healthcare professionals, including sleep specialists, neurologists, and physiotherapists. By understanding the complex relationship between vertigo and sleep disorders, healthcare providers can offer tailored treatment plans that address the unique needs of each individual, ultimately improving their quality of life.
Samsung App Awakening: Tips to Revive Your Sleeping Apps
You may want to see also

Management Strategies: Techniques to manage vertigo symptoms during sleep, such as positional therapy
Vertigo, a sensation of spinning or feeling off-balance, can indeed disrupt sleep and cause frequent awakenings. For individuals prone to vertigo, the experience of sudden dizziness during the night can be particularly distressing. Fortunately, several management strategies can help mitigate these symptoms and improve sleep quality. One effective approach is positional therapy, which involves manipulating body position to alleviate vertigo.
Positional therapy is based on the principle that certain body positions can trigger or exacerbate vertigo symptoms. By understanding these triggers, individuals can learn to adjust their sleeping position to minimize discomfort. For instance, sleeping on your back may cause vertigo symptoms due to the pressure on the inner ear, which can be a common trigger. In this case, side sleeping is often recommended as a more comfortable alternative.
To implement positional therapy, start by experimenting with different sleeping positions. Lie down and observe how your body feels in various orientations. You might find that certain positions, like sleeping on your left side, provide relief from vertigo. This is because this position allows the inner ear to drain naturally, reducing the likelihood of vertigo episodes. Similarly, using extra pillows to support your body and maintain an elevated head position can also help.
Additionally, creating a sleep-friendly environment can further enhance the management of vertigo. Ensure your bedroom is quiet, dark, and at a comfortable temperature. Consider using earplugs or white noise machines to block out sudden sounds that might trigger vertigo. A consistent sleep schedule is also crucial, as it helps regulate your body's internal clock and can reduce the frequency of vertigo episodes.
Incorporating these management strategies into your bedtime routine can significantly improve your sleep experience. While it may take some time to find the most effective positions and techniques for your specific needs, the benefits of better sleep and reduced vertigo symptoms are well worth the effort. Remember, managing vertigo during sleep is a process of self-discovery, and finding the right approach for you is key to achieving a more restful night's sleep.
The Ultimate Guide to Falling Asleep and Waking Up Restored
You may want to see also

Medical Interventions: Exploring treatments and therapies to alleviate vertigo and improve sleep
Vertigo, a sensation of spinning or feeling off-balance, can indeed disrupt sleep and cause insomnia. It is a symptom often associated with inner ear issues, brain disorders, or cardiovascular problems. When vertigo strikes, it can be challenging to fall asleep or stay asleep, leading to fatigue and a decreased quality of life. Fortunately, several medical interventions and therapies are available to help manage and alleviate vertigo, ultimately improving sleep patterns.
One common approach to treating vertigo is through vestibular rehabilitation therapy (VRT). This specialized form of physical therapy focuses on retraining the brain to compensate for the inner ear's imbalance. VRT involves a series of exercises designed to improve balance, reduce dizziness, and enhance the brain's ability to process spatial orientation. Patients typically work with a trained therapist who guides them through specific movements and maneuvers to stimulate the vestibular system. These exercises can include head movements, walking in different directions, and performing tasks that challenge balance. VRT has shown promising results in reducing vertigo symptoms and improving overall function, allowing individuals to experience better sleep quality.
Medications also play a crucial role in managing vertigo and its impact on sleep. Antihistamines, such as diphenhydramine, can be prescribed to reduce the sensation of dizziness and promote sleep. Additionally, anti-anxiety medications may be recommended to address the psychological aspects of vertigo, as anxiety and stress can exacerbate symptoms. In some cases, doctors might prescribe vestibular suppressants or antiemetics to control nausea and vomiting associated with vertigo, which can further interfere with sleep. It is essential to consult a healthcare professional to determine the most suitable medication and dosage for individual needs.
For individuals with vertigo caused by inner ear disorders, such as benign paroxysmal positional vertigo (BPPV), specific maneuvers can be performed to dislodge the calcium crystals that cause the spinning sensation. These maneuvers, often taught by a specialist, involve rapid head movements and specific positioning. By manipulating the inner ear's balance, these techniques can effectively reduce vertigo episodes and improve sleep. Moreover, for more severe cases or when other treatments fail, surgical interventions might be considered to address the underlying cause of vertigo.
In addition to medical interventions, lifestyle modifications can significantly contribute to managing vertigo and enhancing sleep. Maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a comfortable sleep environment are essential. Patients are often advised to avoid sudden movements or activities that trigger vertigo symptoms, especially before bedtime. Staying hydrated, managing stress through relaxation techniques, and incorporating a healthy diet can also positively impact vertigo management and overall sleep quality.
Mastering the Art of Waking Up from Light Sleep
You may want to see also
Frequently asked questions
Yes, vertigo can occur during sleep, and it is often associated with sleep disorders or conditions affecting the inner ear and balance. Sleep-related vertigo may be caused by positional changes, sleep apnea, or conditions like benign paroxysmal positional vertigo (BPPV), which can trigger symptoms like dizziness and a spinning sensation.
Vertigo can significantly impact sleep quality. The symptoms of vertigo, such as dizziness and balance issues, can make it difficult to fall asleep or stay asleep. Frequent awakenings due to vertigo episodes can lead to sleep deprivation, leaving individuals feeling tired and unrefreshed during the day.
Absolutely. Vertigo can be a symptom of various sleep disorders, including sleep apnea and restless leg syndrome. Sleep apnea, for instance, involves pauses in breathing during sleep, which can cause frequent awakenings and lead to vertigo-like symptoms. Treating the underlying sleep disorder is essential to managing vertigo effectively.
Yes, certain sleep positions can exacerbate vertigo symptoms. For individuals with conditions like BPPV, lying down or changing positions rapidly can sometimes trigger vertigo episodes. Side sleeping or using a pillow to elevate the head may help reduce the occurrence of vertigo during sleep.
Managing vertigo during sleep involves a combination of strategies. Maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a comfortable sleep environment can help. For severe cases, consulting an ENT specialist or a neurologist is advisable to identify the cause and develop a treatment plan. They may recommend specific exercises, medications, or therapies to alleviate vertigo symptoms and improve sleep quality.