Sleep onset REM periods (SOREMPs) refer to REM (rapid eye movement) sleep that occurs within 15 minutes of falling asleep. SOREMPs are a highly specific indicator of narcolepsy in the absence of another sleep disorder. However, they have low sensitivity, meaning that a normal REM onset latency does not rule out narcolepsy. SOREMPs can also be observed in patients with obstructive sleep apnea, depressive patients, and healthy individuals under certain conditions, such as shift work or partial sleep deprivation. The appearance of SOREMPs is influenced by various factors, including circadian rhythm, body temperature, and sleep duration.
| Characteristics | Values |
|---|---|
| Definition | Sleep onset REM periods (SOREMPs) are REM (rapid eye movement) sleep periods that happen within 15 minutes of falling asleep. |
| Linked Condition | If you have SOREMPs, it may mean you have narcolepsy. |
| REM Latency | ≤15 minutes |
| Prevalence | Rare (1.0% in general sleep clinic samples) |
| Sensitivity | Low (6.7%) |
| Specificity | High (99.5%) |
What You'll Learn
- Sleep onset REM periods are REM sleep periods that occur within 15 minutes of falling asleep
- SOREMPs are indicative of narcolepsy
- SOREMPs are also observed in patients with sleep apnea
- SOREMPs are affected by REM propensity in the circadian rhythm in normal nocturnal sleep
- SOREMPs may be observed in people experiencing isolated sleep paralysis

Sleep onset REM periods are REM sleep periods that occur within 15 minutes of falling asleep
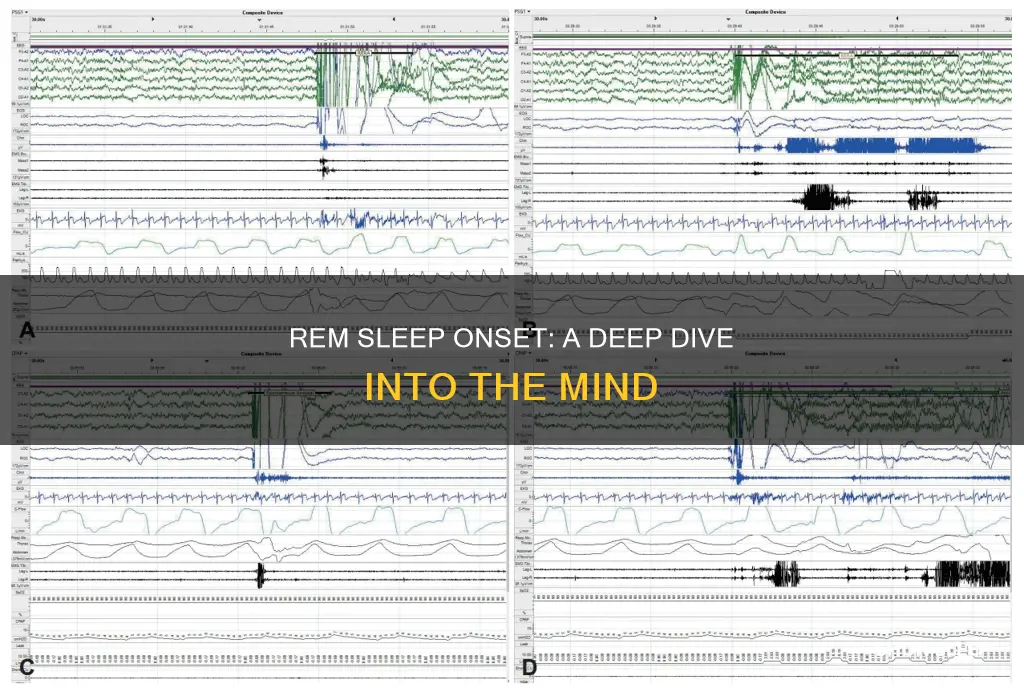
Sleep onset REM periods, or SOREMPs, are periods of REM (rapid eye movement) sleep that occur within 15 minutes of falling asleep. This is characterised by a REM latency of 15 minutes or less, and can be observed in people with narcolepsy. SOREMPs can also be observed in those with depression, and even in healthy individuals under certain conditions.
SOREMPs are a highly specific indicator of narcolepsy, but they are not sensitive, meaning that a normal REM onset latency does not preclude a diagnosis of narcolepsy. Indeed, the presence of SOREMPs can be used as part of the diagnostic criteria for narcolepsy. However, SOREMPs are not always present in people with narcolepsy, and other factors such as gender, sleepiness, nocturnal REM sleep latency, and oxygen desaturation may also be predictive of the condition.
SOREMPs can also be observed in patients with obstructive sleep apnea (OSA), which can cause diagnostic uncertainty. Furthermore, certain factors such as working night shifts or having a positive airway pressure titration can increase the prevalence of PSG SOREMPs. Therefore, it is important to rule out other sleep disorders and ensure adequate sleep timing and duration before conducting sleep testing.
In healthy individuals, SOREMPs may be observed in those who follow non-24-hour sleep/wake schedules, such as shift workers, or those who experience isolated sleep paralysis. SOREMPs may also occur following sleep interruption, with a higher prevalence observed in short sleepers compared to long sleepers.
Detecting REM Sleep: Are You Getting Enough?
You may want to see also

SOREMPs are indicative of narcolepsy
Sleep-onset REM periods (SOREMPs) are REM (rapid eye movement) sleep periods that occur within 15 minutes of falling asleep. SOREMPs are indicative of narcolepsy.
Narcolepsy is a sleep disorder characterised by excessive sleepiness, fragmented nocturnal sleep, and, in some cases, REM-sleep intrusion into wakefulness. The prevalence of narcolepsy is rare, with an estimated rate of between 0.02% and 0.2% for narcolepsy with cataplexy, and 0.2% for narcolepsy without cataplexy. Due to its low prevalence, narcolepsy is often misdiagnosed as other sleep/wake conditions.
The presence of SOREMPs is a highly specific indicator of narcolepsy. A SOREMP within 15 minutes of sleep onset is a highly specific finding in the absence of another sleep disorder. However, SOREMPs have low sensitivity, meaning that a normal REM onset latency does not preclude a diagnosis of narcolepsy. Nevertheless, the presence of SOREMPs, particularly in conjunction with other clinical symptoms of narcolepsy, can provide strong evidence of the disorder.
The International Classification of Sleep Disorders, Third Edition (ICSD-3) allows for a SOREMP during PSG (polysomnography) to count toward one of the two or more SOREMPs required on the subsequent MSLT (Multiple Sleep Latency Test) for a diagnosis of narcolepsy. The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) suggests that a SOREMP during PSG is sufficient to confirm a narcolepsy diagnosis without requiring an MSLT.
In children and adolescents, the presence of a nocturnal SOREMP is highly suggestive of narcolepsy with cataplexy and provides further evidence of REM sleep dysregulation in this condition. The specificity of an nSOREMP for detecting narcolepsy with cataplexy in this age group is high at 97.3%, although the sensitivity is moderate at 54.8%.
In summary, while SOREMPs are not always present in people with narcolepsy and are not sufficient on their own to confirm a diagnosis, they are a highly specific indicator of the disorder. The presence of SOREMPs, particularly when combined with other clinical symptoms and diagnostic tests, can provide strong evidence to support a narcolepsy diagnosis.
How Sleep Stages Affect Body Recovery
You may want to see also

SOREMPs are also observed in patients with sleep apnea
Sleep-onset REM periods (SOREMPs) refer to REM (rapid eye movement) sleep that occurs within 15 minutes of falling asleep. SOREMPs are indicative of narcolepsy, but they are also observed in patients with sleep apnea.
In patients with sleep apnea, SOREMPs are associated with several factors, including male sex, sleepiness, short nocturnal latency to sleep, short nocturnal latency to REM sleep, low percentage of stage 2 sleep, high AHI (apnea/hypopnea index), low minimal oxygen saturation, and high AHIN (apnea/hypopnea index during non-REM sleep). The presence of SOREMPs in patients with sleep apnea can cause diagnostic uncertainty, as it may indicate the presence of narcolepsy. However, the occurrence of SOREMPs in patients with sleep apnea may be due to neurophysiological mechanisms rather than any underlying abnormality.
The presence of SOREMPs in patients with sleep apnea can be influenced by various factors. One potential explanation is nocturnal, selective REM sleep deprivation due to the tendency of sleep apnea to be more severe during this sleep stage. Additionally, sleepiness and apnea severity have been found to correlate with the likelihood of SOREMPs. Other factors such as age, sex, and nocturnal sleep architecture may also play a role, but their influence has not been extensively studied.
The occurrence of SOREMPs in patients with sleep apnea raises questions about the underlying pathophysiological mechanisms. While the strong associations found in observational studies suggest a possible causal relationship, further research is needed to confirm this. The presence of SOREMPs in these patients highlights the importance of considering multiple factors when interpreting sleep study results and making a diagnosis.
Unlocking REM Sleep: Tips for Better Rest
You may want to see also

SOREMPs are affected by REM propensity in the circadian rhythm in normal nocturnal sleep
Sleep-onset REM periods (SOREMPs) are REM (rapid eye movement) sleep periods that occur within 15 minutes of falling asleep. SOREMPs are often indicative of narcolepsy.
SOREMP appearance rates are affected by REM propensity in the circadian rhythm of normal nocturnal sleep. REM latency usually ranges from 60 to 120 minutes, but under certain conditions, it may be less than 25 minutes, which is when it is known as a SOREMP. The major factor that affects REM propensity is the circadian rhythm of REM sleep, which is linked to body temperature rhythm.
In a study by Sasaki et al. (2000), the nocturnal sleep of 16 subjects was interrupted in either the second or fourth cycle of sleep. The SOREMP% was found to be 58.1% in the early condition and 87.5% in the late condition, a significant difference. The body temperature dropped at the second sleep onset in both conditions, but the drops did not differ significantly. The study concluded that SOREMP% was affected by circadian variations in REM propensity, but there was no linear relationship between SOREMP% and body temperature drop.
The appearance of SOREMPs is also affected by individual factors such as being a short sleeper. Short sleepers tend to have a higher REM sleep pressure or REM propensity, which can lead to an increased likelihood of SOREMPs. Additionally, SOREMPs may be observed in individuals with non-24-hour sleep/wake schedules, such as shift workers or those with partial sleep deprivation.
In summary, SOREMPs are influenced by various factors, including circadian rhythm variations, individual differences, and sleep/wake schedules. These factors can interact to contribute to the appearance of SOREMPs, even in the absence of any pathology. Further studies are needed to fully understand the complex interplay of these factors and their impact on SOREMPs.
N-REM Sleep: The Unconscious Half of Our Sleep Cycle
You may want to see also

SOREMPs may be observed in people experiencing isolated sleep paralysis
Sleep-onset REM periods (SOREMPs) refer to
REM Sleep: Brain Growth and Development
You may want to see also
Frequently asked questions
Sleep onset REM periods (SOREMPs) are periods of REM (rapid eye movement) sleep that happen within 15 minutes of falling asleep.
SOREMPs are indicative of narcolepsy.
SOREMPs occur rarely in general sleep clinic samples (<1.0%) but are highly specific for the diagnosis of narcolepsy.