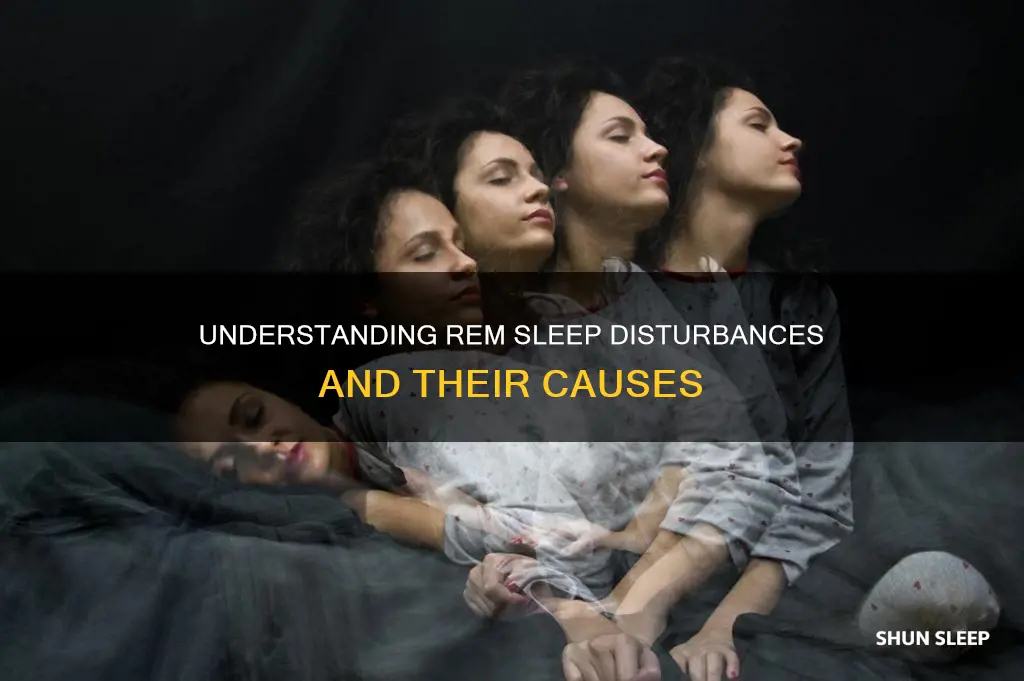
REM sleep behaviour disorder (RBD) is a sleep disorder that causes people to act out their dreams, often violently, while remaining asleep. This can result in injury to themselves or their bed partner. During the REM stage of sleep, the body usually experiences temporary paralysis, known as atonia, while the brain remains active and dreaming. However, for those with RBD, this paralysis does not occur, allowing them to physically act out their dreams. RBD is a parasomnia, a sleep disorder that involves undesirable physical events or experiences that disrupt sleep.
| Characteristics | Values |
|---|---|
| Type of sleep disorder | Parasomnia |
| Sleep stage | REM sleep |
| Behaviour | Acting out dreams, including violent behaviour |
| Vocalisations | Talking, shouting, screaming, laughing, swearing |
| Movements | Punching, kicking, grabbing, jumping out of bed, muscle twitches |
| Awareness | Unaware of actions during sleep |
| Recall | Able to recall dreams upon waking |
| Age of onset | Over 50; average age of 61 |
| Prevalence | 1% of the general population; 2% of over-50s |
| Risk factors | Neurodegenerative disorders, antidepressants, alcohol, sedatives, age, gender (9x more common in men) |
| Treatment | Medication (melatonin, clonazepam), safety measures, lifestyle changes |
What You'll Learn

What is REM sleep?
Sleep is generally divided into two stages: REM (rapid eye movement) and NREM (non-rapid eye movement). During the REM stage, your eyes move rapidly, and your brain activity is similar to its activity when you're awake. This is when most of your dreams occur.
Sleep cycles last between 90 and 120 minutes, with each cycle including three stages of NREM sleep and a stage of REM sleep. After falling asleep, you enter NREM sleep first, followed by a shorter period of REM sleep, and then the cycle starts over again. A typical night involves alternating between four or five sleep cycles.
During the REM stage, your closed eyes move rapidly in different directions, and your brain activity increases. Your heart rate, blood pressure, and breathing increase to levels close to what you experience when you are awake. Your muscles become temporarily paralysed, preventing you from acting out your dreams.
REM sleep is important for brain health and function. It aids in brain development, particularly the central nervous system, which includes the brain and spinal cord. This may explain why newborns require a significant amount of REM sleep. Additionally, REM sleep helps with memory consolidation, problem-solving abilities, and mood regulation. Research suggests that inadequate REM sleep may increase the risk of dementia.
The amount of REM sleep needed changes as we age. Newborns spend about half their sleep time in REM sleep, which gradually decreases to around 20% by age 20 and further reduces to about 17% by age 80.
Weed, REM Sleep, and You: Understanding the Complex Relationship
You may want to see also

What is REM sleep behaviour disorder?
REM sleep behaviour disorder (RBD) is a parasomnia that causes people to act out their dreams. During normal REM sleep, the body experiences temporary paralysis, known as atonia, while the brain shows activity similar to wakefulness. However, for those with RBD, this paralysis does not occur, allowing them to physically act out their dreams.
RBD symptoms include minor movements of the limbs, more pronounced body movements such as punching, flailing, kicking, sitting up in bed, or jumping out of bed, and vocalisations including talking, yelling, or screaming. The dreams associated with RBD are often intense, vivid, and frightening, and may involve being chased or attacked. The person may wake up during the attack and vividly recall the dream that corresponds to the physical activity.
RBD is relatively rare, affecting between 0.5 to 1% of adults, and is more common in men and adults over 50. It is often associated with other neurological conditions, particularly alpha-synucleinopathies such as Parkinson's disease, Lewy body dementia, and multiple system atrophy. RBD often precedes the development of these neurodegenerative diseases by several years. In addition, RBD has been linked to antidepressant use, traumatic brain injury, and post-traumatic stress disorder.
The diagnosis of RBD requires confirmation by an in-laboratory sleep study (polysomnography) with video recording, which helps to identify abnormal behaviours during REM sleep and exclude other sleep disorders. Treatment for RBD involves a combination of lifestyle changes, medication, and injury prevention techniques. Melatonin is the preferred first-line medication, while clonazepam has proven effective in reducing symptoms for 50-80% of individuals with RBD.
SSRIs and REM Sleep: A Complex Relationship
You may want to see also

What are the symptoms of REM sleep behaviour disorder?
REM sleep behaviour disorder (RBD) is a parasomnia that involves dream enactment behaviour. This is associated with a loss of muscle atonia during REM sleep, which can lead to violent sleep-related movements that may result in injury to oneself or one's sleeping partner.
The symptoms of RBD include:
- Talking
- Yelling
- Punching
- Kicking
- Sitting up
- Jumping out of bed
- Arm flailing
- Grabbing
These dream-enacting behaviours can occur at any frequency, from nightly to annually, and usually appear at least 90 minutes after falling asleep. The person may wake up during an episode and be able to recall the dream that corresponds to the physical activity.
RBD is usually seen in middle-aged to elderly people and is more common in men.
Understanding the Link Between REM Sleep and Learning
You may want to see also

How is REM sleep behaviour disorder diagnosed?
REM sleep behaviour disorder (RBD) is a parasomnia, a sleep disorder characterised by abnormal behaviours during sleep. Diagnosis of RBD can be made by a doctor or sleep physician, and there are several criteria that must be met for a person to receive a diagnosis of RBD.
Firstly, the patient must have experienced repeated episodes of acting out their dreams, with physical movements and vocalisations that correspond to what is taking place in the dream. These episodes can include minor movements of the limbs, as well as more pronounced body movements such as punching, kicking, sitting up in bed, or jumping out of bed. Vocalisations can include talking, yelling, or screaming.
Secondly, it must be confirmed that these episodes are occurring during REM sleep. This can be done through an in-laboratory polysomnogram (an overnight sleep study) or by examining the patient's clinical history. Polysomnography will monitor the patient's breathing, eye movements, arm and leg movements, brain and heart activity, and blood oxygen levels. It is also common to videotape the exam to record any dream enactment behaviour.
Thirdly, it must be confirmed that the episodes are characterised by sleep without atonia (lack of muscle paralysis). This can be done through polysomnography, which will show the absence of muscle paralysis during REM sleep.
Finally, other potential causes must be ruled out, such as another sleep or mental health disorder, medication side effects, substance abuse, or alcohol withdrawal. A physical and neurological exam will be conducted to rule out other potential causes, and the doctor will look for symptoms of Parkinson's disease, which has been known to coexist with RBD. If the patient sleeps with a partner, the doctor may ask them to describe any dream enactment behaviours they have observed.
Understanding REM Sleep: Is It Bad To Interrupt?
You may want to see also

What causes REM sleep behaviour disorder?
REM sleep behaviour disorder (RBD) is a parasomnia that involves dream enactment behaviour and is associated with a loss of muscle tone during REM sleep. This can lead to serious harm to the individual and their sleeping partners. The exact cause of RBD is unknown, but it has been linked to several factors, including:
- Neurodegenerative diseases: RBD is strongly linked to neurodegenerative diseases, particularly Parkinson's disease, dementia with Lewy bodies, and multiple system atrophy. Symptoms of RBD may precede these disorders by several years.
- Antidepressant use: RBD has been associated with the use of certain types of antidepressants, including serotonin reuptake inhibitors (e.g., fluoxetine), tricyclic antidepressants (e.g., imipramine), and monoamine oxidase inhibitors (e.g., phenelzine).
- Alcohol and drug withdrawal: Acute forms of RBD can occur during withdrawal from alcohol, sedative-hypnotic drugs, or antidepressants.
- Narcolepsy: RBD has been found in a significant percentage of individuals with narcolepsy type I.
- Age and gender: RBD is more common in middle-aged to elderly individuals and is more prevalent in men.
- Traumatic brain injury: Studies have suggested an association between RBD and traumatic brain injury (TBI).
- Post-traumatic stress disorder: There is some evidence linking RBD and post-traumatic stress disorder (PTSD).
- Congenital and neurodevelopmental disorders: RBD has been associated with certain congenital and neurodevelopmental disorders.
- Wilson disease, cerebellar degeneration, and autoimmune encephalitis: There have been reports of RBD in patients with these conditions.
- Antibodies against IgLON5: A novel association has been found between RBD and antibodies against IgLON5, a neuronal cell adhesion molecule.
Magnesium's Effect on REM Sleep: A Natural Solution?
You may want to see also
Frequently asked questions
REM stands for rapid-eye movement sleep. It is a stage of sleep where the eyes move rapidly under closed eyelids, and the body experiences temporary paralysis while the brain is active and dreaming. This is the stage of sleep where vivid dreams occur.
A disturbance in REM sleep is a sleep disorder called REM Sleep Behavior Disorder (RBD). It is characterised by physical and/or vocal enactment of dreams while in the REM stage of sleep. The person is unaware that they are acting out their dreams.
The symptoms of RBD include minor limb movements, more pronounced body movements such as punching or kicking, and vocalisations like talking or shouting. These episodes can occur once or multiple times during the night and can develop suddenly or gradually.
The primary goal of treatment is to create a safe sleeping environment for the patient and their bed partner. This can include removing hazardous objects from the bedroom and implementing padding on the floor and furniture. Medication such as melatonin or clonazepam may also be prescribed in severe cases.