Sleep paralysis is a parasomnia, a category of sleep disorder that involves abnormal movements, behaviours, and emotions during sleep. There are two types of parasomnias: REM-related and non-REM-related. Sleep paralysis is considered a REM parasomnia as it is linked to the rapid eye movement (REM) stage of the sleep cycle. During REM sleep, the eyes move quickly, and vivid dreaming occurs, but the body's muscles are relaxed to prevent movement. This is known as REM atonia. However, during sleep paralysis, the individual wakes up suddenly from REM sleep, regaining awareness while their muscles are still relaxed. This results in a temporary inability to move or speak, with the person remaining conscious throughout the episode.
| Characteristics | Values |
|---|---|
| Type of parasomnia | REM-related parasomnia |
| Stage of sleep | Between sleep and wakefulness |
| State of the body | Unable to move or speak |
| State of the mind | Conscious |
| Duration | A few seconds to a few minutes |
| End of episode | Ends on its own or when someone moves, touches or speaks to the person |
| Frequency | Once in a person's life or repeatedly over their lifetime |
| Age | Can occur at any age |
| First symptoms | Often show up in childhood, adolescence or young adulthood |
| Episodes | More frequent in the 20s and 30s |
| Risk factors | Sleep deprivation, irregular sleep schedule, mental health conditions, certain medications, substance use disorder |
What You'll Learn

Sleep paralysis is a parasomnia
Sleep paralysis is a temporary inability to move or speak that occurs directly after falling asleep or upon waking up. During an episode of sleep paralysis, you are conscious but unable to move or speak. Sleep paralysis is often accompanied by hallucinations and a sensation of suffocation. It is considered a parasomnia because it is linked to the REM stage of the sleep cycle, during which the eyes move quickly and vivid dreaming occurs. While standard REM sleep involves atonia (muscle relaxation) and dreaming, these typically end upon waking up. However, during sleep paralysis, you may regain awareness while your muscles remain relaxed, resulting in a temporary sense of paralysis.
There are two types of sleep paralysis: isolated sleep paralysis and recurrent sleep paralysis. Isolated sleep paralysis refers to one-off episodes that are not connected to an underlying diagnosis of narcolepsy or other sleep disorders. Recurrent sleep paralysis involves multiple sleep paralysis episodes over time and can be associated with narcolepsy. In many cases, these two types overlap, resulting in a condition called recurrent isolated sleep paralysis (RISP), which involves ongoing instances of sleep paralysis without an association with narcolepsy.
Episodes of sleep paralysis can last from a few seconds to a few minutes and usually end on their own or when someone moves, touches, or speaks to the affected individual. While there is no treatment to stop an episode during its occurrence, treatment options are available to reduce the frequency of episodes. These include medications that prevent individuals from reaching the REM stage of sleep or treating underlying mental health conditions or sleep disorders. Improving sleep hygiene, such as maintaining a consistent sleep schedule and creating a comfortable sleep environment, can also help reduce the risk of sleep paralysis.
The Intriguing Link Between ______ and REM Sleep
You may want to see also

It occurs during the REM stage of sleep
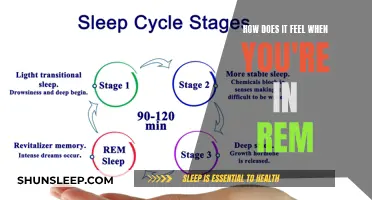
Sleep paralysis is a parasomnia, which is an abnormal behaviour that occurs during sleep. Parasomnias are grouped by the stage of sleep in which they happen, and there are two main stages of sleep: non-rapid eye movement (Non-REM) sleep and rapid eye movement (REM) sleep.
Sleep paralysis occurs during the REM stage of sleep. During REM sleep, the eyes move quickly, and vivid dreaming occurs, but the muscles of the body are relaxed to reduce movement. This muscle relaxation is controlled by the brain and is called REM atonia. The purpose of atonia is to keep you from acting out your dreams, and it typically ends when you wake up. However, during sleep paralysis, you wake up suddenly from REM sleep, regaining awareness even as your muscles are still relaxed, in atonia. For this reason, sleep paralysis may feel like temporary paralysis.
Sleep paralysis is a temporary inability to move or speak that occurs directly after falling asleep or upon waking up. During an episode, you are conscious but unable to move or speak. Episodes last from a few seconds to a few minutes and usually end on their own, or when someone moves or touches you, or speaks to you. Making an intense effort to move can also end an episode.
In addition to atonia, people often experience hallucinations during episodes of sleep paralysis. These hallucinations can be frightening or cause anxiety. They fall into three categories: intruder hallucinations, chest pressure hallucinations, and vestibular-motor (V-M) hallucinations.
Dreaming Beyond REM Sleep: What Does It Mean?
You may want to see also

It involves hallucinations
Sleep paralysis is a parasomnia, a category of sleep disorder that involves abnormal movements, behaviours, emotions, perceptions, and dreams that occur while falling asleep, sleeping, between sleep stages, or during arousal from sleep. Parasomnias are dissociated sleep states that occur during the transitions between wakefulness, non-rapid eye movement (Non-REM) sleep, and rapid eye movement (REM) sleep.
Sleep paralysis occurs when an individual is stuck between sleep phases, unable to move or speak, but conscious and aware of their surroundings. It is considered a REM parasomnia as it is linked to the REM stage of the sleep cycle. During REM sleep, the eyes move quickly, and vivid dreaming occurs, but the muscles of the body are relaxed to reduce movement. This muscle relaxation is called REM atonia and is controlled by the brain. However, during sleep paralysis, an individual may suddenly regain awareness while their muscles are still relaxed, resulting in a temporary sense of paralysis.
Sleep paralysis often involves hallucinations, which can be frightening and cause anxiety. These hallucinations typically fall into three categories:
Intruder Hallucinations
Intruder hallucinations involve the perception of a dangerous person or presence in the room, such as an intruder. These hallucinations can be terrifying and cause intense fear and anxiety.
Chest Pressure Hallucinations
Also known as incubus hallucinations, individuals experiencing these hallucinations may feel a sense of pressure on their chest, as if someone is sitting on them, or sensations of being choked or suffocated. These hallucinations often occur alongside intruder hallucinations, intensifying the sense of danger and distress.
Vestibular-Motor (V-M) Hallucinations
V-M hallucinations can include feelings of movement, such as flying, or out-of-body sensations. These hallucinations can create a sense of detachment from one's physical body and a distorted perception of reality.
It is important to note that these hallucinations are distinct from typical dreams. They can be hypnagogic hallucinations, occurring when falling asleep, or hypnopompic hallucinations, occurring when waking up.
While the exact cause of sleep paralysis is unknown, it is often associated with sleep disorders, irregular sleep schedules, mental health conditions, certain medications, and substance use. Improving sleep hygiene and addressing underlying sleep problems and mental health conditions can help reduce the frequency and severity of sleep paralysis episodes.
SSRIs and REM Sleep: A Complex Relationship
You may want to see also

It can be isolated or recurrent
Sleep paralysis is a parasomnia, which is a sleep disorder that involves abnormal and undesirable physical events or experiences that disrupt sleep. Parasomnias are grouped by the stage of sleep in which they happen. There are two main stages of sleep: non-rapid eye movement (Non-REM) sleep and rapid eye movement (REM) sleep. Sleep paralysis is considered a REM parasomnia.
There are two types of sleep paralysis: isolated sleep paralysis and recurrent sleep paralysis. Isolated sleep paralysis refers to one-off episodes that are not connected to an underlying diagnosis of narcolepsy, a neurological disorder that prevents the brain from properly controlling wakefulness. Recurrent sleep paralysis involves multiple sleep paralysis episodes over time and can be associated with narcolepsy.
In many cases, these two types overlap and are described as recurrent isolated sleep paralysis (RISP), which involves ongoing instances of sleep paralysis in someone who does not have narcolepsy. Sleep paralysis can be isolated or recurrent, and it can occur at any age, although symptoms often first appear in childhood, adolescence, or young adulthood. Episodes may become more frequent in a person's 20s and 30s.
Isolated sleep paralysis episodes are not linked to an underlying condition, whereas recurrent sleep paralysis is associated with multiple episodes over time and may be related to narcolepsy. Recurrent sleep paralysis can be a sign of an underlying neurological issue, such as narcolepsy, which requires medical attention.
Episodes of sleep paralysis can be distressing and cause anxiety, fear, or emotional distress. They can last from a few seconds to a few minutes and usually end on their own or when someone moves, touches, or speaks to the affected person. Sleep paralysis is not considered dangerous in isolation, but recurrent or bothersome episodes can lead to negative thoughts about sleep, reduced sleep time, and anxiety around bedtime, resulting in sleep deprivation and potential health consequences.
REM Sleep: Strategies for Soothing Toddler's Slumber
You may want to see also

It can be prevented by improving sleep hygiene
Sleep paralysis is a parasomnia, or abnormal behaviour that occurs during sleep. It is a temporary condition in which a person is conscious but unable to move or speak, and it happens when the body is stuck between sleep phases, usually between wakefulness and sleep. While it is not dangerous, it can be a frightening experience and cause emotional distress.
Sleep paralysis can be prevented by improving sleep hygiene. Here are some ways to improve sleep hygiene and reduce the risk of sleep paralysis:
- Maintain a set sleep schedule: Go to bed and wake up at the same time every day, including on weekends. A consistent sleep schedule helps regulate your body's sleep-wake cycle and can improve the quality of your sleep.
- Create a comfortable sleep environment: Make your bedroom dark, cool, and quiet. These conditions are optimal for sleep and can help you fall asleep more easily.
- Reduce distractions: Avoid using electronic devices such as phones, tablets, e-readers, and computers before bedtime. The blue light emitted by these devices can interfere with your sleep hormones, making it harder to fall asleep.
- Relax before bed: Engage in relaxing activities such as taking a bath, reading, or listening to soothing music. This can help reduce stress levels and prepare your mind and body for sleep.
- Try different sleeping positions: If you sleep on your back, consider trying a different position. Research has found a correlation between sleeping on your back and sleep paralysis.
- Improve sleep habits: Ensure you are getting adequate sleep, typically 7-9 hours per night for adults. Also, try to reduce stress, especially before bedtime, and curb substance use, such as alcohol and nicotine, which can interfere with sleep.
By improving sleep hygiene and making lifestyle changes, you can reduce the risk of experiencing sleep paralysis and improve your overall sleep quality.
REM Sleep: Psychology's Window to the Unconscious Mind
You may want to see also
Frequently asked questions
Sleep paralysis is a temporary loss of muscle control that occurs just after falling asleep or before waking up. During an episode, a person is conscious but unable to move or speak.
Sleep paralysis often involves hallucinations or a feeling of suffocation. People also report distressing emotions like panic or helplessness during episodes.
Sleep paralysis is considered a REM parasomnia as it is linked to the rapid eye movement (REM) stage of the sleep cycle.