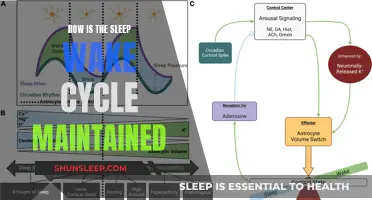
Sleep-wake homeostasis is a fundamental process that regulates our sleep-wake cycles, ensuring we get the rest we need. It involves a delicate balance between sleep pressure and the body's natural circadian rhythms. This homeostatic mechanism monitors our sleep patterns and adjusts our internal clocks to maintain optimal sleep and wakefulness. When we are awake, our bodies accumulate a sleep drive, which increases as we stay alert. Conversely, during sleep, this drive is reduced, promoting wakefulness. The intricate interplay between our biological clocks and the sleep-wake homeostasis system orchestrates the timing of our sleep and wake states, influencing our overall health and well-being. Understanding this process is crucial to comprehending the complexities of sleep and its impact on our daily lives.
| Characteristics | Values |
|---|---|
| Sleep-Wake Homeostasis Theory | The concept suggests that sleep drives accumulate during wakefulness, and this drive is proportional to the time spent awake. When the drive reaches a certain threshold, sleep occurs to reset the system. |
| Homeostatic Regulation | This process involves the body's internal mechanisms that monitor and adjust sleep-wake cycles. It helps maintain optimal sleep duration and quality. |
| Sleep Pressure Build-up | As individuals stay awake, a sleep drive or pressure builds up, which is influenced by various factors like sleep need, circadian rhythm, and recent sleep history. |
| Sleep Drive Intensity | The intensity of the sleep drive varies with the time of day and individual differences. It is highest in the early evening and decreases during the night. |
| Sleep-Wake Cycle | The cycle is regulated by the body's internal biological clock (circadian rhythm) and external cues like light and temperature. Homeostasis helps synchronize this cycle. |
| Sleep Onset | Homeostasis plays a role in initiating sleep by promoting sleepiness and reducing wakefulness. It helps individuals fall asleep when the sleep drive is strong enough. |
| Sleep Depth and Quality | Homeostatic processes influence the depth and quality of sleep. Adequate sleep pressure ensures deeper, more restorative sleep stages. |
| Sleep-Wake Transition | The transition between wakefulness and sleep is regulated by homeostatic and circadian mechanisms. It ensures a smooth shift into sleep when needed. |
| Individual Differences | Sleep-wake homeostasis can vary among individuals due to genetic factors, age, and lifestyle. Some people may have a higher or lower threshold for sleep drive. |
| Sleep Disorders | Dysregulation of sleep-wake homeostasis is linked to various sleep disorders, such as insomnia, narcolepsy, and sleep apnea. |
What You'll Learn
- Sleep-wake cycle regulation: The body's internal clock and its response to light
- Homeostatic sleep drive: Accumulation of sleep pressure during wakefulness
- Sleep-promoting neurotransmitters: GABA and adenosine's role in sleep initiation
- Sleep-wake feedback loops: Interactions between the brain and the body
- Sleep homeostasis disruption: Effects of sleep deprivation and shift work

Sleep-wake cycle regulation: The body's internal clock and its response to light
The human body's sleep-wake cycle is a complex process regulated by an internal biological clock, often referred to as the circadian rhythm. This internal clock is a natural, self-sustaining mechanism that operates on a roughly 24-hour cycle, influencing various physiological processes, including sleep and wakefulness. The primary factor that synchronizes this internal clock with the external environment is light, particularly the daily cycle of daylight and darkness.
Our bodies have specialized cells in the retina of the eye called photoreceptors, which detect light and send signals to the brain. One type of photoreceptor, known as intrinsically photosensitive retinal ganglion cells (ipRGCs), plays a crucial role in regulating the circadian rhythm. These cells are sensitive to light, especially a specific wavelength of blue light, and they transmit information about the light-dark cycle to the brain's master clock, located in the hypothalamus.
When light enters the eyes, it triggers a cascade of events. The ipRGCs are activated, and they signal the brain to suppress the production of melatonin, a hormone that promotes sleep. This response is essential for maintaining alertness during the day. Conversely, in the absence of light, especially during the night, the ipRGCs are less active, allowing melatonin levels to rise, preparing the body for sleep. This light-dependent mechanism ensures that the body's internal clock remains synchronized with the external day-night cycle.
The brain's master clock, known as the suprachiasmatic nucleus (SCN), plays a critical role in coordinating this process. It receives input from the ipRGCs and other sensory systems, and it generates the circadian rhythm, which influences the timing of sleep and wakefulness. The SCN also regulates the release of hormones, such as cortisol and adrenaline, which promote alertness and energy during the day and help prepare the body for rest at night.
In summary, the sleep-wake cycle is tightly regulated by the body's internal clock, which is primarily influenced by light exposure. The ipRGCs in the retina detect light and signal the brain to adjust hormone levels, promoting wakefulness during the day and sleep at night. This intricate process ensures that the body's circadian rhythm aligns with the natural day-night cycle, optimizing energy levels and overall health. Understanding this mechanism is crucial in comprehending the impact of light on our sleep patterns and the potential disruptions caused by artificial light exposure, especially in modern urban environments.
Migraine's Impact: Can It Interrupt Your Sleep?
You may want to see also

Homeostatic sleep drive: Accumulation of sleep pressure during wakefulness
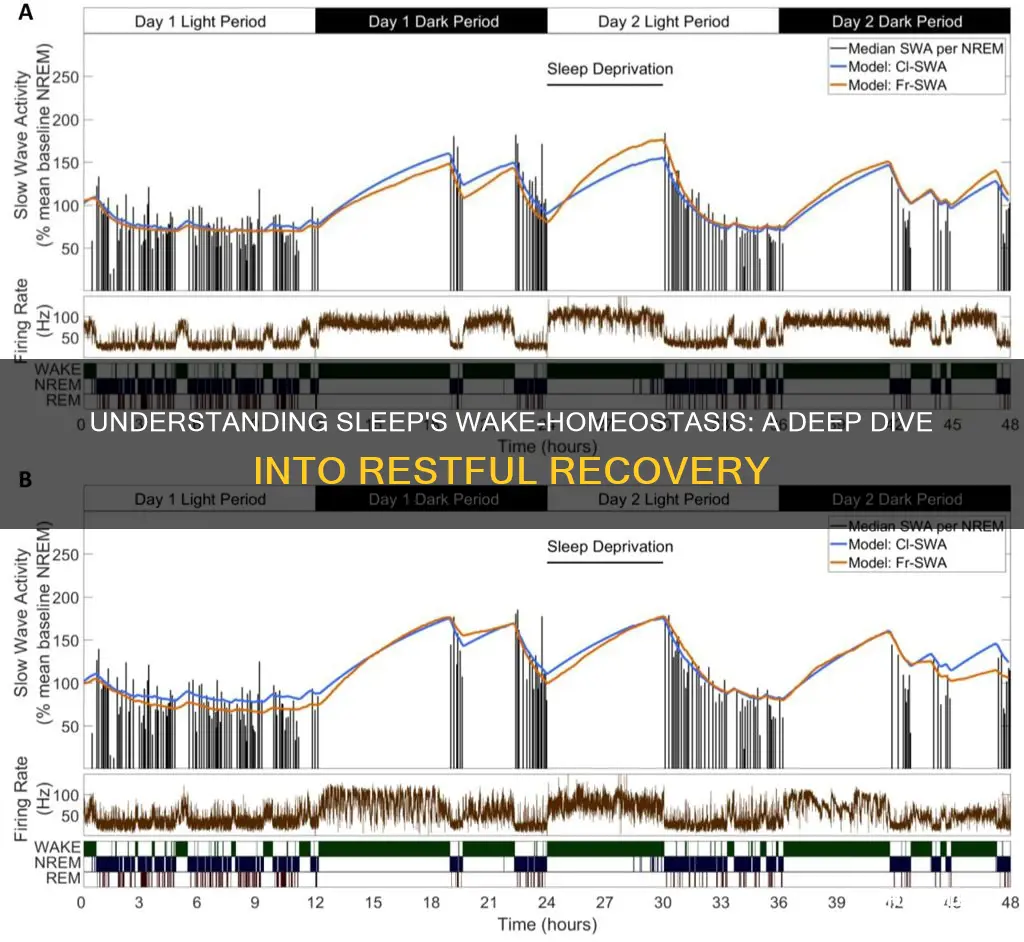
The concept of homeostatic sleep drive is fundamental to understanding why we feel the need to sleep and how our bodies regulate sleep-wake cycles. This drive is essentially a biological mechanism that accumulates sleep pressure during periods of wakefulness, ensuring that we eventually feel the urge to rest. It's like a built-in alarm system that monitors our body's energy needs and triggers sleep when necessary.
During wakefulness, our bodies engage in various processes to maintain energy levels. One crucial aspect is adenosine, a neurotransmitter that plays a significant role in sleep-wake regulation. As we stay awake, adenosine levels in the brain gradually increase. This accumulation of adenosine is a direct indicator of our body's sleep pressure. It binds to specific receptors, particularly in the brainstem, which is responsible for regulating sleep and wakefulness. The higher the adenosine levels, the stronger the drive to sleep becomes.
This homeostatic process is a slow and gradual one. It doesn't trigger an immediate sleep response but rather builds up over time. The longer we remain awake, the more adenosine accumulates, and the stronger the sleep drive becomes. This is why you might feel more tired as the day progresses, especially after a long period of activity. Your body is accumulating sleep pressure, and it's preparing to initiate sleep when an opportunity arises.
The accumulation of sleep pressure is not just about feeling tired; it's a complex physiological process. It involves the activation of specific brain regions and the release of hormones that prepare the body for rest. For example, the brain produces cytokines, which are proteins that promote sleep and reduce inflammation. These cytokines are released in response to the increasing sleep drive, further emphasizing the body's need for rest.
Understanding this homeostatic mechanism is essential as it highlights the importance of maintaining a consistent sleep schedule. Disrupting this balance can lead to sleep disorders and impaired cognitive function. By recognizing the gradual accumulation of sleep pressure, we can appreciate the need for adequate sleep and make informed decisions to ensure our bodies receive the rest they require.
Overcoming Early Bird Challenges: Waking Up at 9
You may want to see also

Sleep-promoting neurotransmitters: GABA and adenosine's role in sleep initiation
Sleep initiation is a complex process that involves the interplay of various physiological and biochemical mechanisms. Among these, neurotransmitters play a crucial role in promoting sleep by modulating the activity of neurons and influencing the sleep-wake cycle. Two key neurotransmitters that contribute significantly to sleep initiation are Gamma-Aminobutyric Acid (GABA) and Adenosine.
GABA, a inhibitory neurotransmitter, is known for its role in calming the nervous system and reducing neuronal excitability. In the context of sleep, GABA acts as a sleep-promoting neurotransmitter by inhibiting the release of excitatory neurotransmitters like glutamate. This inhibition helps to lower brain activity, making it easier for the body to transition into a state of relaxation and sleep. Research has shown that GABA receptors are particularly active in brain regions associated with sleep regulation, such as the hypothalamus and the brainstem. When GABA binds to its receptors, it triggers a series of intracellular events that ultimately lead to the release of sleep-inducing hormones, such as somatotropin-releasing hormone (STRH) and growth hormone (GH).
Adenosine, another key player in sleep initiation, is a neurotransmitter that accumulates in the brain during wakefulness and promotes sleepiness. It does so by binding to specific adenosine receptors, primarily A1 and A2A receptors, which are widely distributed in the brain. As adenosine levels increase during the day, it triggers a cascade of events that prepare the body for sleep. One of the primary effects of adenosine is the modulation of the brain's arousal centers, particularly the hypothalamus and the brainstem. By binding to these receptors, adenosine inhibits the release of excitatory neurotransmitters, thereby reducing brain activity and promoting a state of calmness. This process is essential for the body's natural sleep drive, often referred to as the homeostatic sleep drive, which ensures that we feel the need to sleep when our bodies have been deprived of adequate rest.
The interaction between GABA and adenosine is particularly intriguing. As adenosine levels rise, they enhance GABA's inhibitory effects, further promoting sleep. This synergy between these two neurotransmitters helps to explain why they are both essential for initiating and maintaining sleep. During the day, when adenosine levels are low, GABA's role in inhibiting excitatory neurotransmitters becomes more pronounced, helping to maintain a calm and relaxed state. However, as the day progresses and adenosine levels increase, the combined action of GABA and adenosine becomes even more critical in preparing the body for sleep.
In summary, GABA and adenosine are key neurotransmitters that work in concert to initiate and promote sleep. GABA's inhibitory action on excitatory neurotransmitters helps to calm the nervous system, while adenosine's accumulation during wakefulness binds to specific receptors, modulating brain activity and promoting sleepiness. The interplay between these two neurotransmitters is a fundamental aspect of the sleep-wake homeostasis, ensuring that we can effectively transition from a state of wakefulness to a state of restorative sleep. Understanding these mechanisms can provide valuable insights into the treatment of sleep disorders and the development of strategies to improve sleep quality.
Revive Your Battery: Simple Steps to Wake a Slumbering Lithium-Ion
You may want to see also

Sleep-wake feedback loops: Interactions between the brain and the body
The sleep-wake cycle is a complex process regulated by a delicate balance of internal and external factors, creating a feedback loop that ensures our bodies and minds are prepared for the day's challenges and rested for the night's repair. This intricate dance between the brain and the body is a fundamental aspect of sleep-wake homeostasis. At the core of this process is the brain's biological clock, a network of neurons that acts as a master regulator. This internal clock is influenced by external cues, primarily light, which is detected by specialized cells in the retina. When light enters the eyes, it triggers a cascade of events, suppressing the production of melatonin, a hormone that promotes sleep. This reduction in melatonin levels signals to the body that it's time to be awake and alert.
As we stay awake, our brain's activity increases, leading to a state of hyperarousal. This heightened state is characterized by increased heart rate, blood pressure, and body temperature. The brain's reward centers are also activated, promoting behaviors that encourage wakefulness, such as seeking food, social interaction, and physical activity. This feedback loop is crucial for maintaining alertness during the day. However, as time passes, the body's need for sleep becomes increasingly apparent. The brain detects signs of fatigue, such as decreased alertness and cognitive performance, and responds by initiating the sleep drive.
During sleep, the body undergoes a series of restorative processes. One of the key mechanisms is the regulation of hormone levels. For instance, growth hormone, essential for cell regeneration and repair, is released primarily during deep sleep. Additionally, the brain consolidates memories and processes information, ensuring that the day's experiences are encoded and stored. This process is vital for learning and cognitive function. As sleep progresses, the body's core temperature drops, and melatonin levels rise, reinforcing the sleep-wake cycle.
The sleep-wake feedback loop is a dynamic process, constantly adjusting to internal and external demands. It is influenced by various factors, including age, lifestyle, and environmental conditions. For example, consistent exposure to bright light during the day can reset the biological clock, promoting better sleep at night. Similarly, irregular sleep patterns can disrupt the natural rhythm, leading to a desynchronized sleep-wake cycle. Understanding this feedback loop is essential for promoting healthy sleep habits and managing sleep disorders. By recognizing the intricate interactions between the brain and the body, we can develop strategies to optimize sleep, enhance overall well-being, and improve daily functioning.
Gentle Strategies: Waking Your Newborn for Feeding Time
You may want to see also

Sleep homeostasis disruption: Effects of sleep deprivation and shift work
Sleep homeostasis is a fundamental process that regulates our sleep-wake cycles, ensuring we get the necessary amount of sleep to function optimally. It is a complex biological mechanism that maintains a balance between sleep and wakefulness, allowing us to stay alert during the day and prepare for rest at night. This homeostatic process is influenced by various internal and external factors, and its disruption can have significant consequences for our overall health and well-being.
When we are awake, our body accumulates a 'sleep debt' or a physiological need for sleep. This debt is a result of the body's natural circadian rhythm, which is a 24-hour cycle that regulates our sleep-wake cycles. During the day, as we engage in activities and consume caffeine or other stimulants, our body's sleep drive increases, and we may feel more alert. However, as time passes, this sleep drive intensifies, and we become more susceptible to sleepiness. This is where sleep homeostasis comes into play. The body's sleep drive is counterbalanced by a 'sleep pressure' or a state of sleepiness that builds up over time, which is regulated by the homeostatic process.
Sleep deprivation, whether acute or chronic, significantly disrupts this delicate balance. When we consistently fail to get sufficient sleep, our body's sleep drive remains high, while the sleep pressure is reduced. This imbalance leads to excessive daytime sleepiness, impaired cognitive function, and a decreased ability to perform tasks that require focus and concentration. Over time, chronic sleep deprivation can result in more severe consequences, including metabolic disorders, cardiovascular issues, and a weakened immune system.
Shift work, a common practice in many industries, also poses a significant challenge to sleep homeostasis. Workers who perform night shifts or rotating schedules often experience a misalignment between their natural circadian rhythms and the required work hours. This disruption can lead to a phenomenon known as 'social jet lag,' where the body's internal clock is out of sync with the external environment. As a result, shift workers may struggle to fall asleep during the day, experience reduced sleep quality, and suffer from increased sleepiness and fatigue.
The effects of sleep homeostasis disruption are far-reaching. It can impact an individual's mood, cognitive abilities, and overall health. Research has shown that sleep deprivation and shift work can contribute to the development of mood disorders, such as depression and anxiety. It may also increase the risk of accidents and errors in judgment, particularly in professions that require high levels of alertness, such as transportation and healthcare. Moreover, long-term disruption of sleep homeostasis can lead to chronic health issues, including obesity, diabetes, and cardiovascular diseases.
Understanding the impact of sleep homeostasis disruption is crucial for promoting better sleep hygiene and improving the well-being of individuals affected by sleep deprivation and shift work. Strategies such as maintaining a consistent sleep schedule, creating a relaxing sleep environment, and practicing good sleep hygiene can help mitigate the effects of sleep deprivation. For shift workers, implementing gradual schedule adjustments, utilizing nap opportunities, and promoting a healthy lifestyle can contribute to better sleep and overall health.
The Science Behind the Struggle: Why Waking Up is So Tough
You may want to see also
Frequently asked questions
Sleep-wake homeostasis refers to the biological process that regulates our sleep-wake cycles and maintains a balance between sleep and wakefulness. It is a fundamental mechanism that ensures we get enough sleep to function optimally.
The body's internal clock, known as the circadian rhythm, plays a crucial role in sleep-wake homeostasis. It is influenced by external cues, primarily light, which help regulate the release of hormones like melatonin and cortisol. During the day, light exposure suppresses melatonin, promoting alertness. At night, reduced light triggers melatonin production, making us feel sleepy.
Disruption to sleep-wake homeostasis can occur due to various factors such as shift work, jet lag, or chronic sleep deprivation. When this balance is disturbed, it can lead to a phenomenon called sleep debt, where the body accumulates a deficit of sleep. This can result in increased sleepiness, impaired cognitive function, mood disturbances, and a higher risk of developing sleep disorders.
To enhance sleep-wake homeostasis, it is essential to prioritize sleep hygiene. This includes maintaining a consistent sleep schedule, creating a relaxing bedtime routine, ensuring a comfortable sleep environment, and limiting exposure to screens before bed. Regular physical activity and a healthy diet can also positively impact sleep quality.
Yes, exposure to natural light during the day, especially in the morning, can help reset the circadian rhythm. A short nap in the early afternoon can also be beneficial, but it's important not to oversleep. Gradually adjusting sleep and wake times, especially when traveling across time zones, allows the body to naturally readjust its internal clock.