Obstructive sleep apnea (OSA) is a sleep disorder that can occur during REM sleep, and it is defined by the presence of episodes of apnea or hypopnea during this stage. OSA is characterised by partial (hypopnea) or complete (apnea) reduction of airflow during sleep, caused by pharyngeal obstruction. This can cause a case of hypoxia and sleep discontinuity.
REM sleep is one of the deepest stages of sleep, and it is associated with dreaming and memory consolidation. During REM sleep, your eyes move rapidly, your heart rate increases, and your breathing becomes irregular. In contrast to other stages of sleep, your brain is highly active during this stage.
OSA during REM sleep is a common disorder, and it has been linked to several health outcomes, including hypertension, poor glycemic control, and cardiovascular disease. The prevalence of OSA during REM sleep is estimated to be between 14% and 36%, and it is more common in females.
The treatment for OSA during REM sleep is positive airway pressure (PAP) therapy, which helps to keep the airway open while the patient sleeps. However, the current standard treatment may not be sufficient to treat all apnea episodes during REM sleep, and further investigation is needed to determine the best approach for managing this disorder.
| Characteristics | Values |
|---|---|
| --- | --- |
| Prevalence | 10-37% |
| Occurrence | Predominantly or exclusively during REM sleep |
| Severity | Mild to moderate |
| Associated Conditions | Sleepiness, hypertension, poor glycemic control, cardiovascular disease |
| Treatment | CPAP therapy |
What You'll Learn

REM sleep and the effects of sleep apnea
Obstructive Sleep Apnea (OSA) is a highly prevalent sleep disorder characterised by partial or complete upper airway collapse, causing interrupted breathing during sleep. This can prevent the body from getting enough oxygen and lead to chronic sleep deprivation, as well as other mental and physical health issues if left untreated.
REM (rapid eye movement) sleep is one of the deepest stages of sleep, accounting for 20-25% of total sleep time. During REM sleep, the eyes move rapidly, the heart rate increases, and breathing becomes irregular. Unlike other sleep stages, the brain is highly active during REM sleep, and brain waves are more variable.
OSA can occur during REM sleep, and this is known as REM-related OSA. During REM sleep, there is an increased tendency for upper airway collapse due to decreased genioglossus muscle tone. REM-related OSA is defined by the presence of apnoea or hypopnoea predominantly or exclusively during REM sleep. The prevalence of REM-related OSA varies depending on the criteria used for diagnosis and is estimated to be between 14% and 36%. It is more common in women than in men and tends to occur in those with mild to moderate OSA overall.
The clinical significance of REM-related OSA is not yet well understood, and it is unclear whether it is associated with similar neurocognitive and cardiometabolic health outcomes as non-stage-specific OSA. However, some studies have found associations between REM-related OSA and specific health outcomes.
REM-related OSA has been linked to:
- Increased risk of hypertension, particularly in those with prevalent cardiovascular disease.
- Impaired glucose metabolism and poor glycemic control.
- Daytime sleepiness and reduced quality of life.
- Neurocognitive and cardiometabolic adverse outcomes.
The gold standard treatment for moderate to severe OSA is Continuous Positive Airway Pressure (CPAP) therapy, which can be effective in treating REM-related OSA and improving related symptoms. However, the current recommended duration of CPAP therapy may not be sufficient to treat REM-related OSA, as it occurs predominantly in the latter half of the sleep period. Therefore, there is a need for further research and standardised definitions to guide the diagnosis and management of REM-related OSA.
Diphenhydramine: Preventing REM Sleep or Just a Myth?
You may want to see also

REM sleep and the treatment of sleep apnea
Obstructive sleep apnea (OSA) is a highly prevalent condition that has been associated with cardiovascular morbidity and mortality, impaired glucose metabolism, and daytime functional impairment. During REM sleep, healthy individuals experience higher sympathetic activity and cardiovascular instability than during non-rapid eye movement (NREM) sleep. This effect is even more pronounced in patients with OSA.
OSA during REM sleep is associated with a higher risk of cardiovascular issues, including hypertension, and metabolic complications such as insulin resistance and impaired glucose metabolism. It has also been linked to an impairment of human spatial navigational memory.
OSA during REM sleep is quite prevalent, especially in women, younger individuals, and those with mild to moderate OSA. However, the clinical significance of REM OSA remains controversial. While some studies have reported a link between OSA during REM sleep and hypersomnolence, several large cross-sectional and longitudinal studies have found no association with excessive daytime sleepiness.
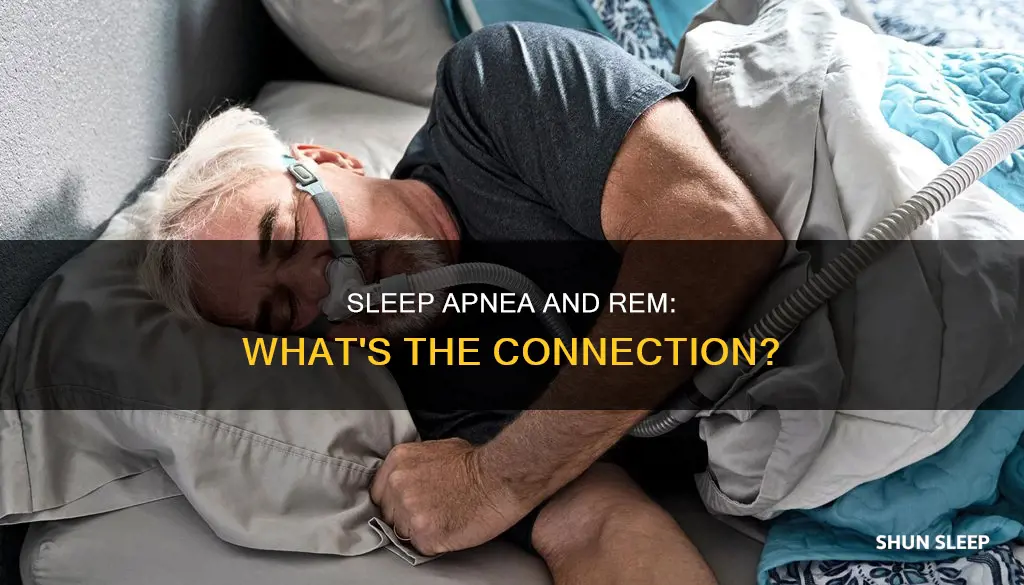
The treatment of OSA during REM sleep is challenging due to the poor adherence to continuous positive airway pressure (CPAP) therapy, which is often recommended for OSA. CPAP therapy typically covers only the first half of the sleep period, leaving most REM sleep untreated. Alternative treatments, such as oral appliances, may be more effective for OSA during REM sleep, but more research is needed.
Clinicians should emphasize the need for prolonged CPAP usage that includes the early morning hours before awakening in patients with REM-predominant OSA. Further research is required to establish the optimal duration of CPAP therapy for treating REM OSA and to evaluate patients with REM OSA who have an overall normal apnea-hypopnea index.
Understanding REM Sleep Disorders: Causes and Treatments
You may want to see also

REM sleep and the diagnosis of sleep apnea
Obstructive sleep apnea (OSA) is a sleep disorder in which a person's breathing stops and starts repeatedly while they sleep. This can prevent the body from getting enough oxygen and cause chronic sleep deprivation, leading to other mental and physical health issues if left untreated. OSA can occur in both non-rapid eye movement (NREM) sleep and REM sleep, or be limited to REM sleep. During REM sleep, the airway is most prone to collapse, and respiratory events are usually longer and more desaturating than in NREM sleep.
The prevalence of REM-related OSA varies depending on the criteria used to define it and the population studied, but it is generally estimated to be between 10% and 36%. It is more common in women than in men and is often identified in those with mild to moderate OSA.
The clinical significance of REM-related OSA is not yet well-defined, and it is unclear whether it is associated with similar neurocognitive and cardiometabolic morbidity as non-stage-specific OSA. Some studies have found that REM-related OSA is associated with daytime sleepiness, while others have not. However, there is growing evidence that REM-related OSA may be independently associated with hypertension, impaired glucose metabolism, and cardiovascular disease, particularly in those with pre-existing cardiovascular disease.
The gold standard treatment for moderate to severe OSA is continuous positive airway pressure (CPAP) therapy, which helps to keep the airway open during sleep. CPAP therapy has been shown to improve sleepiness, fatigue, mood, and overall functional status in patients with REM-related OSA, and their compliance with CPAP is similar to patients without REM-related OSA. However, the current definition and treatment of REM-related OSA are not standardized, and there is a lack of consensus on whether patients with this diagnosis should be treated if their overall apnea-hypopnea index does not meet the threshold for clinical diagnosis of OSA.
Further research is needed to determine the clinical significance of REM-related OSA and to standardize its diagnosis and treatment.
Understanding and Overcoming REM Sleep Challenges
You may want to see also

REM sleep and the prevalence of sleep apnea
Obstructive sleep apnea (OSA) is a highly prevalent condition, affecting 5%–24% of males and 1%–9% of females. It is characterised by daytime fatigue, sleepiness, snoring, and witnessed apnoeas. These signs and symptoms are the result of partial (hypopnea) or complete (apnea) reduction of airflow during sleep caused by pharyngeal obstruction.
OSA can occur in both rapid eye movement (REM) and non-REM sleep or be limited to REM sleep. During REM sleep, the upper airway is most prone to collapse due to REM sleep atonia. Respiratory events are usually longer and more desaturating in REM than in non-REM sleep. The prevalence of REM OSA is higher in women than in men and REM OSA usually occurs in the context of mild-moderate OSA.
The clinical significance of REM-related OSA is not well-defined, and it remains unclear if REM-related OSA is associated with similar neurocognitive and cardiometabolic morbidity as non-stage specific OSA. However, recent studies have shown that REM OSA is independently associated with prevalent and incident hypertension, non-dipping of nocturnal blood pressure, increased insulin resistance, and impairment of human spatial navigational memory.
The gold standard of treatment for moderate to severe OSA continues to be continuous positive airway pressure (CPAP) therapy. Patients with REM-related OSA show improvement in sleepiness, fatigue, mood, and overall functional status following CPAP therapy. However, the treatment of REM-related OSA is further complicated by the different definitions used for diagnosis and the lack of consensus on whether patients with this diagnosis should be treated if their overall apnea-hypopnea index does not meet the threshold for the clinical diagnosis of OSA.
Unlocking REM Sleep: The Memory Storage Mystery
You may want to see also

REM sleep and the symptoms of sleep apnea
Obstructive sleep apnea (OSA) is a sleep disorder in which a person's breathing stops and starts repeatedly while they sleep. This can prevent the body from getting enough oxygen and cause chronic sleep deprivation, which can lead to other mental and physical health issues. OSA can occur in both rapid eye movement (REM) and non-REM sleep or be limited to REM sleep, when the upper airway is most prone to collapse due to REM sleep atonia. Respiratory events are usually longer and more desaturating in REM than in non-REM sleep.
OSA during REM sleep is associated with a higher incidence of a composite cardiovascular endpoint, but only in those with prevalent cardiovascular disease. REM sleep–related OSA has also been independently associated with prevalent and incident hypertension and impairments in glucose metabolism.
The clinical significance of REM-related OSA is not well-defined, and it remains unclear if REM-related OSA is associated with similar neurocognitive and cardiometabolic morbidity as non-stage-specific OSA.
The gold standard of treatment for moderate to severe OSA continues to be CPAP therapy. Patients with REM-related OSA show improvement in sleepiness, fatigue, mood, and overall functional status following CPAP therapy, and their compliance with CPAP is similar to patients who do not have episodes of apnea restricted to REM sleep.
REM sleep is an essential part of a healthy sleep cycle. Disrupted by sleep disorders, the loss of this important sleep stage can leave you sleep-deprived. REM sleep disorders and sleep apnea can prevent individuals from achieving this critical level of sleep, which can also cause long-term physical and mental health issues.
REM Sleep: Can It Hurt Your Eyes?
You may want to see also
Frequently asked questions
REM sleep is a stage of sleep associated with dreaming and memory consolidation. It is one of the deepest stages of sleep. During REM sleep, your eyes move rapidly behind your closed eyes, your heart rate speeds up, and your breathing becomes irregular. In contrast to other stages of sleep, your brain is highly active during this stage, and your brain waves become more variable.
Sleep apnea can interrupt and even prevent the REM sleep stage. The frequent closing of the airway causes frequent awakenings throughout the night so that the body never fully slips into the REM stage of sleep. This can cause sleep deprivation, which can leave you with a foggy brain in the morning as your body never fully consolidates the memory during the night.
The best treatment for obstructive sleep apnea continues to be PAP therapy. Using a CPAP machine, patients receive a steady flow of pressurized air through a mask to help keep the airway open while they sleep. For REM sleep disorders specifically, your doctor may also recommend medications if PAP therapy is not enough.