Sleep-wake disorders, such as insomnia, hypersomnia, and circadian rhythm sleep-wake disorders, are complex conditions that can significantly impact an individual's quality of life. While the exact causes of these disorders are not fully understood, research suggests that both psychological and genetic factors play a role in their development and manifestation. Understanding the interplay between these factors is crucial for developing effective treatment strategies and improving the management of sleep-wake disorders. This paragraph aims to explore the psychological and genetic influences on sleep-wake disorders, highlighting the need for a comprehensive approach to their treatment and management.
| Characteristics | Values |
|---|---|
| Definition | Sleep-wake disorders are a group of conditions that affect the normal sleep-wake cycle, causing difficulties in falling asleep, staying asleep, or waking up. |
| Types | Insomnia, narcolepsy, sleep apnea, restless leg syndrome, and circadian rhythm sleep-wake disorders. |
| Causes | Genetic factors, environmental influences, psychological conditions, and lifestyle choices. |
| Genetic Influence | Research suggests a genetic component, with certain genes potentially predisposing individuals to sleep disorders. |
| Psychological Factors | Stress, anxiety, depression, and other mental health issues can contribute to sleep problems. |
| Environmental Triggers | Irregular sleep schedules, exposure to light at night, caffeine consumption, and certain medications. |
| Treatment Approaches | Cognitive-behavioral therapy, sleep hygiene education, medication, and lifestyle modifications. |
| Impact | Sleep disorders can lead to fatigue, impaired cognitive function, mood disturbances, and increased risk of health issues. |
| Diagnosis | Sleep studies, questionnaires, and medical history evaluation. |
| Prevention | Consistent sleep routines, regular exercise, and stress management techniques. |
What You'll Learn
- Sleep-Wake Cycle Regulation: Understanding the genetic basis of circadian rhythm disorders
- Psychological Factors: Role of stress, anxiety, and depression in sleep disorders
- Genetic Predisposition: Family history and inherited sleep-wake cycle disruptions
- Neurotransmitter Influence: How genetic variations affect neurotransmitter systems and sleep
- Epigenetic Modifications: Environmental factors and their impact on gene expression in sleep

Sleep-Wake Cycle Regulation: Understanding the genetic basis of circadian rhythm disorders
The regulation of our sleep-wake cycle, or circadian rhythm, is a complex process that involves multiple biological systems, and its understanding has been greatly enhanced by recent genetic research. Circadian rhythm disorders, such as delayed sleep phase syndrome (DSPS) and advanced sleep phase syndrome (ASPS), are conditions where an individual's sleep-wake cycle is misaligned with the natural day-night cycle, causing difficulties in falling asleep or waking up at socially acceptable times. These disorders can significantly impact an individual's quality of life and overall health.
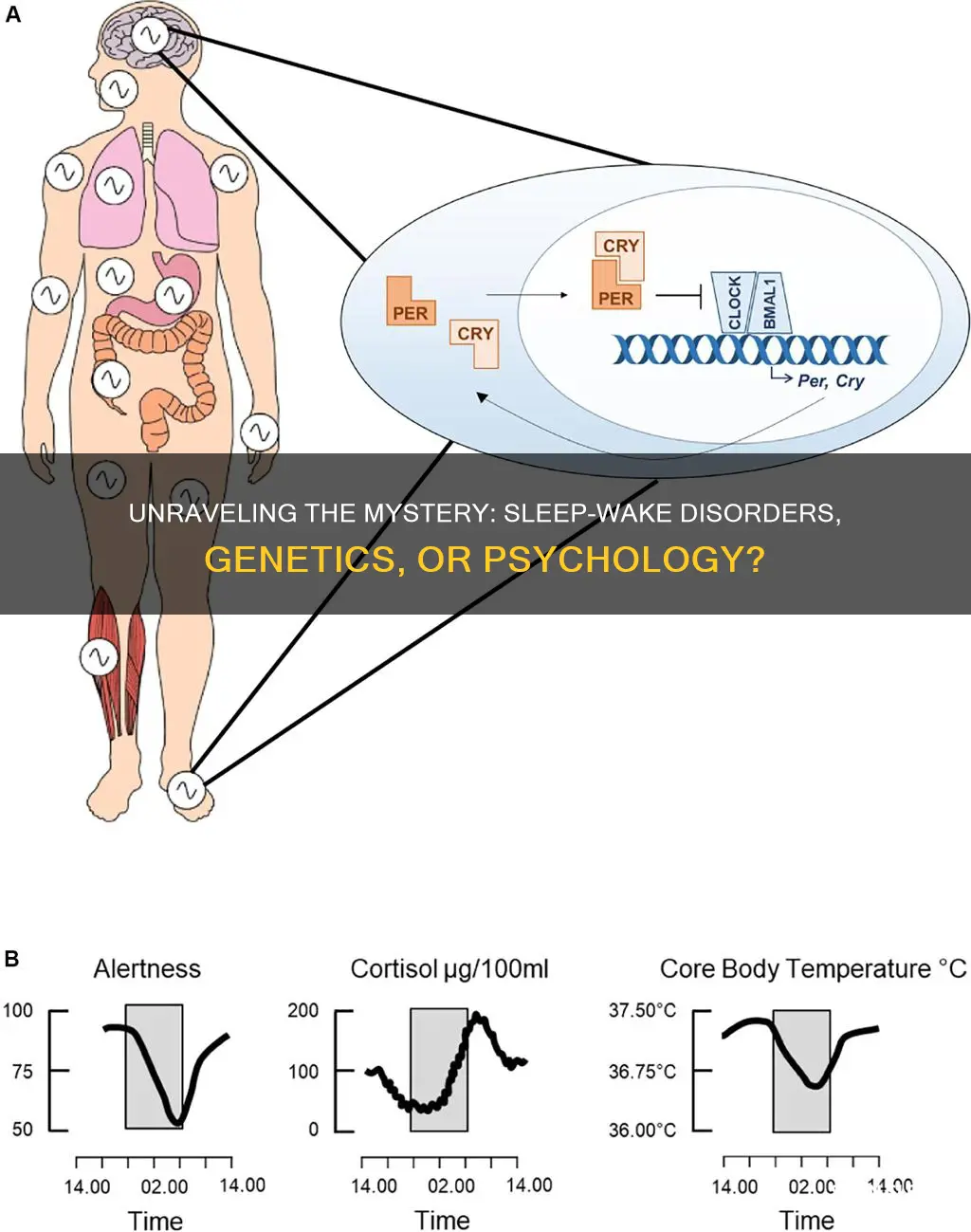
At the core of circadian rhythm regulation are the biological clocks, which are found in various parts of the body, including the brain, heart, and peripheral tissues. The most well-studied biological clock is located in the hypothalamus of the brain, known as the suprachiasmatic nucleus (SCN). The SCN receives light information from the eyes and synchronizes it with the body's internal clock, thus regulating sleep-wake cycles, hormone release, and other physiological processes.
Genetic research has identified several genes that play crucial roles in the regulation of circadian rhythms. One of the most prominent genes is PER (Period), which encodes a protein that forms part of the core clock mechanism in the SCN. Mutations in the PER gene can lead to circadian rhythm disorders, as these mutations disrupt the normal functioning of the biological clock. For example, individuals with DSPS often have a delayed PER gene expression, causing their biological clocks to be out of sync with the external environment. Similarly, ASPS is associated with an advanced PER gene expression, leading to early sleep and wake times.
Other genes, such as CLOCK, BMAL1, and CRY, also contribute to circadian rhythm regulation. These genes form part of a feedback loop that drives the circadian rhythm, and their proper functioning is essential for maintaining a healthy sleep-wake cycle. Research has shown that variations in these genes can influence an individual's susceptibility to circadian rhythm disorders, providing valuable insights into the genetic basis of these conditions.
Understanding the genetic underpinnings of circadian rhythm disorders has significant implications for diagnosis, treatment, and prevention. Genetic testing can help identify individuals at risk of developing these disorders, allowing for early intervention and personalized treatment plans. Additionally, this knowledge can guide the development of targeted therapies, such as light therapy and chronotherapy, which aim to reset the biological clock and improve sleep-wake cycle alignment.
In conclusion, the genetic basis of circadian rhythm disorders is a fascinating area of study, offering valuable insights into the complex regulation of our sleep-wake cycles. By understanding the genes involved in this process, researchers can develop more effective strategies to manage and treat sleep-wake disorders, ultimately improving the quality of life for those affected. Further exploration of these genetic mechanisms will contribute to a more comprehensive understanding of circadian rhythm regulation and its impact on human health.
Feeding Newborns: To Wake or Not to Wake?
You may want to see also

Psychological Factors: Role of stress, anxiety, and depression in sleep disorders
The intricate relationship between psychological factors and sleep disorders is a critical aspect of understanding and treating these conditions. Stress, anxiety, and depression are known to significantly impact sleep patterns, often leading to a vicious cycle of sleep deprivation and worsening mental health. Here's an exploration of these psychological factors:
Stress and Sleep: Chronic stress is a prevalent issue in modern society, and its impact on sleep can be profound. When individuals experience stress, their bodies release stress hormones, such as cortisol, which can disrupt the natural sleep-wake cycle. This disruption often results in difficulty falling asleep, frequent awakenings during the night, and non-restorative sleep. For example, a person with a demanding job and financial worries might find themselves lying awake at night, their minds racing with thoughts about work and money. Over time, this can lead to insomnia, a sleep disorder characterized by persistent difficulty in falling asleep or staying asleep.
Anxiety and Sleep Disorders: Anxiety disorders, including generalized anxiety disorder, panic disorder, and social anxiety disorder, are closely linked to sleep problems. Anxiety can cause a constant state of hyperarousal, making it challenging for individuals to relax and fall asleep. Nighttime anxiety may manifest as insomnia, where individuals experience racing thoughts, worry, and an inability to quiet their minds. Additionally, anxiety disorders can lead to sleep-related breathing issues, such as sleep apnea, where breathing temporarily stops during sleep, causing frequent awakenings and leaving individuals feeling unrefreshed in the morning.
Depression and Sleep Disturbances: Depression is a mood disorder that often co-occurs with sleep disorders. Individuals with depression frequently experience insomnia or hypersomnia (excessive sleepiness). They might have difficulty falling asleep due to racing thoughts and a negative mindset, or they may sleep excessively as a result of low energy and motivation. Depression can also lead to early-morning awakening, where individuals wake up before they feel rested, often feeling sad or hopeless. The relationship between depression and sleep is bidirectional; sleep deprivation can exacerbate depressive symptoms, creating a challenging cycle to break.
Understanding the psychological factors contributing to sleep disorders is essential for developing effective treatment plans. Cognitive-behavioral therapy (CBT) is often used to address these issues, helping individuals manage stress, anxiety, and depression while improving sleep hygiene. Additionally, sleep restriction therapy and stimulus control therapy are techniques employed to regulate sleep patterns and reduce the association between bed and wakefulness. By targeting these psychological aspects, individuals can improve their sleep quality, enhance overall well-being, and potentially mitigate the genetic predispositions to certain sleep wake disorders.
The Ethical Dilemma: Waking Up from Sleep Paralysis
You may want to see also

Genetic Predisposition: Family history and inherited sleep-wake cycle disruptions
The concept of genetic predisposition in sleep-wake disorders is an intriguing aspect of the field, as it delves into the intricate relationship between our genes and our sleep patterns. Research has revealed that certain genetic factors can significantly influence an individual's susceptibility to sleep-wake cycle disruptions, which are often referred to as circadian rhythm disorders. These disorders can manifest in various ways, such as insomnia, hypersomnia, delayed sleep phase syndrome, and advanced sleep phase syndrome, each presenting unique challenges for affected individuals.
Family history plays a pivotal role in understanding the genetic underpinnings of sleep-wake disorders. Studies have consistently shown that individuals with a family history of these disorders are at a higher risk of developing similar conditions. For instance, if a parent or sibling suffers from insomnia or a circadian rhythm disorder, the likelihood of the child experiencing similar sleep issues increases. This familial aggregation suggests a shared genetic component, where specific genes contribute to the development of these disorders.
One of the key genes associated with sleep-wake cycle disruptions is the PER2 gene, which encodes a protein involved in regulating the body's circadian rhythm. Variations in this gene have been linked to delayed sleep phase syndrome, a disorder characterized by a delayed timing of sleep and wakefulness. Individuals with certain PER2 gene variants may have a genetic predisposition to this disorder, making them more susceptible to disruptions in their sleep-wake cycles.
Furthermore, the genetic basis for sleep-wake disorders can be complex and multifaceted. It is believed that multiple genes, each contributing a small effect, may collectively influence the development of these disorders. This genetic architecture could explain why some individuals with a family history of sleep issues do not necessarily develop the condition, while others do. The interplay of various genetic factors and environmental influences is a critical area of research, as it may lead to more personalized approaches to prevention and treatment.
In summary, the genetic predisposition to sleep-wake disorders is evident through family history and inherited sleep-wake cycle disruptions. Understanding the genetic basis of these disorders can provide valuable insights into their development and potentially lead to more targeted interventions. As research progresses, the field of sleep medicine may benefit from a more nuanced understanding of the genetic factors contributing to these complex conditions.
The Ultimate Guide to Falling Asleep and Waking Up Restored
You may want to see also

Neurotransmitter Influence: How genetic variations affect neurotransmitter systems and sleep
The intricate relationship between genetics and sleep is a fascinating area of study, shedding light on how our biological makeup influences our sleep patterns. At the heart of this connection are neurotransmitters, the chemical messengers of the brain, which play a pivotal role in regulating sleep and wakefulness. Neurotransmitters are influenced by genetic variations, and these variations can have a profound impact on an individual's sleep-wake cycles.
One of the key neurotransmitters involved in sleep regulation is GABA (gamma-aminobutyric acid). GABA is an inhibitory neurotransmitter that helps to calm the brain and induce relaxation. Genetic variations in the GABAA receptor, a protein that allows GABA to bind to its receptors, can affect the efficiency of GABA's action. Individuals with certain genetic variants may have a reduced response to GABA, leading to difficulties in falling asleep or staying asleep. This genetic influence on GABA function highlights a potential biological basis for sleep disorders.
Another important neurotransmitter system is the hypothalamic-pituitary-adrenal (HPA) axis, which is crucial for regulating stress responses and sleep-wake cycles. The HPA axis is influenced by cortisol, a hormone that helps regulate energy levels and alertness. Genetic variations in the genes responsible for cortisol production and metabolism can disrupt the normal functioning of the HPA axis. For example, some individuals with specific genetic variants may experience hyperactivity of the HPA axis, leading to increased stress reactivity and potentially impacting their sleep.
Additionally, the serotonin system, which is involved in mood regulation and sleep, is also genetically influenced. Serotonin helps promote sleep and is converted into melatonin, a hormone that regulates sleep-wake cycles. Genetic variations in the genes encoding serotonin-related enzymes can affect serotonin levels and its conversion to melatonin. This disruption in the serotonin-melatonin pathway may contribute to sleep disorders, especially in individuals with certain genetic predispositions.
Understanding the genetic basis of neurotransmitter systems and their impact on sleep provides valuable insights into the development of personalized treatment approaches for sleep disorders. By identifying specific genetic variations, healthcare professionals can tailor interventions to address the underlying biological mechanisms. This knowledge also emphasizes the importance of considering genetic factors when assessing and managing sleep-wake disorders, moving towards more precise and effective clinical practices.
The Awakening: Unlocking the Secrets of Sleep's Second Wind
You may want to see also

Epigenetic Modifications: Environmental factors and their impact on gene expression in sleep
The concept of epigenetic modifications highlights a fascinating interplay between environmental influences and genetic expression, particularly in the context of sleep-wake disorders. These disorders, which encompass conditions like insomnia, hypersomnia, and circadian rhythm sleep-wake disorders, have long been associated with both psychological and biological factors. However, recent research has shed light on the role of epigenetics, suggesting that environmental factors can leave lasting imprints on our genes, potentially influencing sleep patterns and related health outcomes.
Environmental factors, such as exposure to light, diet, and stress, can trigger epigenetic changes, which are modifications that affect gene activity without altering the underlying DNA sequence. One of the most well-studied epigenetic mechanisms is DNA methylation, where methyl groups are added to DNA, often leading to gene silencing. In the context of sleep, research has shown that exposure to artificial light at night, a common modern-day environmental factor, can induce epigenetic changes in the brain. This light exposure may disrupt the natural circadian rhythm, leading to epigenetic modifications that affect genes involved in sleep regulation. For instance, studies have demonstrated that chronic exposure to light at night can result in increased DNA methylation in the promoter region of the PER2 gene, a key regulator of the circadian clock, potentially disrupting the normal sleep-wake cycle.
Another critical environmental factor is diet, which can also influence epigenetic modifications related to sleep. Nutritional components like vitamins, minerals, and certain dietary compounds can impact gene expression. For example, a diet rich in omega-3 fatty acids has been linked to reduced DNA methylation in the promoter of the BDNF gene, which is essential for brain function and mood regulation. This finding suggests that dietary interventions could potentially mitigate sleep-wake disorders by modulating epigenetic markers. Furthermore, the timing of meals and snacks can influence the body's internal clock, potentially affecting the epigenetic landscape related to sleep.
Stress, both physical and psychological, is another significant environmental factor that can leave epigenetic imprints. Chronic stress can lead to increased DNA methylation in genes associated with stress response and immune function. Interestingly, these epigenetic changes may persist even after the stressor is removed, potentially impacting long-term health, including sleep quality. Studies have shown that individuals with insomnia or other sleep disorders often exhibit altered DNA methylation patterns compared to healthy controls, suggesting a potential epigenetic basis for these conditions.
Understanding the role of environmental factors in epigenetic modifications related to sleep has profound implications for both diagnosis and treatment. It opens up new avenues for therapeutic interventions that target these epigenetic changes. For instance, light therapy, which involves controlled exposure to specific wavelengths of light, can help reset the circadian rhythm and potentially reverse epigenetic modifications caused by disrupted sleep. Similarly, dietary modifications and stress management techniques could be used to modulate epigenetic markers, improving sleep quality and overall health.
In conclusion, the study of epigenetic modifications in the context of sleep-wake disorders reveals a dynamic relationship between environmental factors and gene expression. Environmental influences, such as light exposure, diet, and stress, can induce epigenetic changes that impact genes involved in sleep regulation. This knowledge provides a novel perspective on the development and treatment of sleep disorders, emphasizing the importance of considering both psychological and environmental factors in managing these complex conditions. Further research in this area may lead to more personalized and effective therapeutic approaches, ultimately improving the quality of life for individuals affected by sleep-wake disorders.
Overcoming the Struggle: Tips to Wake Up Refreshing
You may want to see also
Frequently asked questions
Sleep-wake disorders, such as insomnia, hypersomnia, and circadian rhythm sleep-wake disorders, can have both psychological and genetic components. While psychological factors like stress, anxiety, and depression often play a significant role in the development and exacerbation of these disorders, genetic predispositions can also contribute. Research suggests that certain genetic variations may increase an individual's susceptibility to sleep disorders, affecting their brain's ability to regulate sleep-wake cycles.
Psychological factors can significantly impact sleep-wake disorders. For example, individuals with insomnia often experience heightened anxiety and stress, which can lead to racing thoughts and difficulty falling asleep. Similarly, conditions like major depressive disorder can disrupt sleep patterns, causing insomnia or hypersomnia. Managing these psychological aspects through therapy, relaxation techniques, and lifestyle changes can be an essential part of treating sleep disorders.
Yes, genetic factors can contribute to the development of sleep-wake disorders. Some studies have identified specific genes associated with sleep-wake regulation, such as those involved in the body's natural circadian rhythm. Genetic variations in these genes can lead to conditions like advanced or delayed sleep-phase syndrome, where individuals have difficulty aligning their sleep schedules with the desired wake times. Additionally, genetic factors may influence the risk of developing insomnia or narcolepsy.
Environmental factors, such as lifestyle choices and external influences, also play a crucial role in sleep-wake disorders. Irregular sleep schedules, excessive screen time before bed, and an inconsistent sleep routine can disrupt the body's natural circadian rhythm. Additionally, environmental stressors, such as noise or light pollution, can impact sleep quality. Addressing these environmental factors through simple changes in daily habits and creating a conducive sleep environment can help manage and improve sleep-wake disorders.